Association between Type 2 Diabetes Mellitus and Moderate to Severe Forms of Covid-19 among Inpatients at the Military Armed Forces Training Hospital Omar BONGO ONDIMBA
Berthe Amélie Iroungou2*, Djibril Diarra1, Jean Raymond Nzenze1, Laurette Guignali Mangouka1
1Internal Medicine Department, Omar Bongo Ondimba Army Training Hospital, Libreville, Gabon
2CIRMF-SSM Joint Research Unit, Libreville, Gabon
*Corresponding author: Berthe Amélie Iroungou, CIRMF-SSM Joint Research Unit, Libreville, Gabon
Received Date: 11 February 2023
Accepted Date: 15 February 2023
Published Date: 17 February 2023
Citation: Iroungou BA, Diarra D, Nzenze JR, Mangouka LG (2023) Association between Type 2 Diabetes Mellitus and Moderate to Severe Forms of Covid-19 among Inpatients at the Military Armed Forces Training Hospital Omar BONGO ONDIMBA. Ann Case Report. 8: 1176. DOI:https://doi.org/10.29011/2574-7754.101176
Abstract
Background: Comorbidities, such as Type 2 diabetes Mellitus, have been identified as high-risk factors for developing moderate or severe COVID-19. In this study, we aimed to explore the epidemiological aspect of COVID-19 in Type 2 diabetes patients in Gabon, Central Africa.
Method: This was a retrospective and descriptive study conducted over a period of 12 months, from September 1, 2020 to December 31, 2021, at the Military Armed Forces Training Hospital Omar BONGO ONDIMBA. The aim of the study was to determine the prevalence and severity of COVID-19 in patients with Type 2 diabetes.
Results: A total of 65 patients were hospitalized in the internal medicine COVID unit and were included in the study. The majority of patients (53.1%) were aged 60 years and older, with a median age of 60 years and a range between 33 and 87 years. The male gender was predominant, accounting for 56.9% of cases. Moderate forms of COVID-19 were observed in 72.3% of patients, with dyspnea being the most common clinical sign (42.6%). Severe forms were observed in 27.7% of patients, and respiratory distress was the dominant clinical sign (50%). A chest CT scan revealed lung damage of more than 50% in these patients. Ketoacidosis, an acute complication of Type 2 diabetes, was observed in 18.5% of patients.
Conclusion: This study highlights the significant impact of Type 2 diabetes on the outcome of COVID-19 infections, increasing the risk of severe forms and resulting in worse vital prognoses for patients. Early detection of diabetes in suspected COVID-19 cases is crucial to mitigate this risk.
Keywords: COVID-19; Moderate and Severe Forms; Type 2 Diabetes; Gabon
Introduction
The Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) is the virus responsible for the coronavirus disease 2019 (COVID-19) outbreak, which first emerged in Wuhan, China in December 2019 and rapidly spread globally. In Africa, the first confirmed case of COVID-19 was reported in February 2020 in Egypt [1]. Gabon was one of the early countries in Central Africa to be affected by COVID-19, after Cameroon and the Democratic Republic of Congo, with its first confirmed case reported on March 13, 2020. One of the prevalent comorbidities in Gabon is Type 2 diabetes, which has been identified as a risk factor for poor prognosis in patients with moderate and severe forms of COVID-19 [2-4]. The aim of the study was to examine the epidemiology of moderate and severe forms of COVID-19 in patients with Type 2 diabetes who were hospitalized in the internal medicine COVID unit at the Military Armed Forces Training Hospital Omar BONGO ONDIMBA (HIA OBO).
Methods
A retrospective and descriptive study was conducted on adult patients (over 18 years old) who were hospitalized for moderate and severe forms of COVID-19 and had a diagnosis of Type 2 diabetes. The study period was 15 months, from September 1, 2020 to December 31, 2021, and all patient records from the Internal Medicine department of the HIA-OBO that met the inclusion criteria were analysed. The definition of moderate and severe forms of COVID-19 was based on the criteria established by the World Health Organization (WHO) [5]. Confirmatory diagnosis of COVID-19 was primarily made through the Reverse Transcriptase-Polymerase Chain Reaction (RT-PCR) test for SARS-CoV-2, conducted on nasopharyngeal swabs to detect the viral genome. Type 2 diabetes mellitus was defined as a fasting blood glucose level greater than 1.26 g/L (7mmol/L) or a blood glucose level at any time of the day greater than 2 g/L (11mmol/L), and this diagnosis was confirmed through repeated testing [6]. In order to accurately diagnose pulmonary abnormalities linked to COVID-19 pneumonia, chest computed tomography (CT) scans without iodinated contrast medium were performed on all patients using a 64-slice Philips Brilliance CT scanner (Philips, Amsterdam, The Netherlands). The scans were sourced from the COVID-Unit HIA Omar BONGO ONDIMBA (HIA OBO), offering valuable information about the disease's evolution.
Data Analysis
The data was analysed using Microsoft Excel 2010 and IBM SPSS Statistics 22 software.
Ethical Considerations
During the ongoing COVID-19 pandemic, all inpatients were fully informed and voluntarily participated in this study after giving their informed consent. To protect patient confidentiality, all data was kept anonymous.
Results
Socio-demographic Characteristics
This study analysed the medical records of 65 out of 80 hospitalized patients who were diagnosed with moderate to severe COVID-19 and had type 2 diabetes. The largest group of patients (50.8%) was aged 60 years or older, followed by those between 41-59 years (40%). The youngest group, 19-40 years, consisted of only 6 patients (9.2%). The median age was 60 years with a range of 33 to 87 years. The majority of patients were male (56.9%) while 43.1% were female.
Type 2 Diabetes Mellitus
In the 65 analysed patient records, we observed that patients with a diagnosis of type 2 diabetes mellitus for at least 5 years made up 24.61% (n=16) of the sample. Those diagnosed between 6 and 9 years accounted for 30.76% (n=20), while those with a diagnosis of over 10 years made up 35.38% (n=23). The remaining 9.23% (n=6) of patients were diagnosed with type 2 diabetes during their hospitalization for COVID-19.
Clinical and paraclinical manifestations of COVID-19 forms
Moderate forms of COVID-19
Out of 65 inpatients with type 2 diabetes, 72.3% (47/65) were diagnosed with moderate forms of COVID-19. The most commonly observed clinical symptom was dyspnea, present in 42.6% of cases, followed by a decline in overall condition in 38.3% of cases, oxygen saturation levels below 92% in 14.9% of cases, and a fever above 38°C in 4.3% of cases. C-reactive protein (CRP) was used as an indicator of inflammation and was elevated in 57.4% of cases. Morphological abnormalities on chest computer tomographic (CT) scan without injection of contrast medium were evaluated at 10-50% of lung lesions in 89.4% of moderate COVID-19 forms. The primary form of pulmonary lesion observed was ground-glass alveolar opacities.
Severe forms of COVID-19
18 patients with type 2 diabetes (27.7% of the sample) were diagnosed with severe forms of COVID-19. Respiratory distress was the most prominent symptom, observed in 50% of cases, followed by shock in 27.8%, heart rate exceeding 30 beats per minute in 11.1%, and altered consciousness as indicated by a Glasgow score below 12 out of 15 in 11.1%. Chest CT scans performed without iodinated contrast medium showed that 77.8% of patients with severe COVID-19 had significant lung involvement, characterized by ground-glass opacities and bilateral sub pleural consolidation, predominantly located in the lung bases. This is depicted in Figures 1A, 1B, 2A, and 2B.
Other manifestations regardless of the form of COVID-19
In addition to the main symptoms of COVID-19, we observed other clinical and laboratory manifestations. Fever was present in the majority of cases (56.9%), while tachycardia was seen in 21.1% of patients. Anaemia was noted in 18.5% (n=12) of patients, hyperleukocytosis in 26.2% (n=17), lymphopenia in 7.7% (n=5), and thrombocytopenia in 13.8% (n=9). Abnormalities in ionic levels were detected in 55.4% (n=36) of patients. In both clinical forms of COVID-19, chest CT-scan mainly highlighted the aspect of sub-pleural condensation in 80% (n=52).
Biological indicators and acute complications of type 2 Diabetes Mellitus and COVID-19
Out of 65 analysed patients, 26 (40%) presented with hyperglycaemia, with glucose levels ranging from 1.26 to 2 g/L. HbA1c levels greater than 8% were seen in 20 (30.8%) of the COVID-19 patients, regardless of the form of the illness. Additionally, elevated ketonuria was observed in 19 (29.2%) cases of COVID-19 associated with type 2 diabetes, as revealed by urine dipstick tests. Of the 65 patients, 17 (26.2%) experienced acute complications related to type 2 diabetes. Ketoacidosis was the most common complication, affecting 18.5% of patients, followed by hyperosmolar syndrome in 6.2% and hyperglycaemia in 1.5% of cases.
Hospitalization Duration in COVID-19 Patients
The duration of hospitalization varied among patients, as shown in the following breakdown: 46.1% (30 patients) had a hospital stay of 1 to 7 days, 35.4% (23 patients) had a hospital stay of 8 to 14 days, 15.4% (10 patients) had a hospital stay of 15 to 29 days, and just 3.1% (2 patients) had a hospital stay of more than 30 days.
Discussion
Socio-demographic aspects
In our study, 50.8% of the COVID-19 patients were elderly (≥60 years). The median age observed was 60 years, with the age range extending from 33 to 87 years? This pattern of an older population being disproportionately affected by COVID-19 has been reported in other countries as well. Waecher. C et al in France observed a similar trend, with the majority of COVID-19 patients being elderly and a median age of 84 years. A similar pattern has also been reported in Guinea [7]. Donamou J. et al in Guinea found that the mean age of COVID-19 patients was 59 ± 14 years, which is similar to the median age observed in our study [8]. The predominance of the elderly among COVID-19 patients can be attributed to the decline in immune defenses associated with aging. Additionally, as noted by various authors, age has been identified as a risk factor for developing moderate to severe forms of COVID-19. In our study, the male gender was predominant among 56.9% of COVID-19 patients. This result aligns with the findings of Donamou J. et al, who reported a male predominance among 79% of COVID-19 patients in their study. Similarly, Waechter C. et al also found a male predominance among COVID-19 patients [7]. Based on our results, it appears that both advanced age and male gender may have a significant impact on the prognosis of moderate to severe forms of COVID-19 in patients with type 2 diabetes [9-11].
Clinical and paraclinical features of COVID-19 forms
Moderate forms of COVID-19
In moderate forms of COVID-19, dyspnea was the most commonly reported clinical sign, accounting for 42.6% of cases. This result was in line with the findings of Zerah L. et al, who reported a similar rate of 45%, while Waechter C. et al reported a lower rate of 25.5% [7,12]. In our study, 57.4% of patients with moderate forms of COVID-19 associated with type 2 diabetes had elevated CRP levels above 50 mg/l [13]. These results suggest that early damage to the lung parenchyma by SARS-CoV-2 and decreased oxygen delivery may be contributing factors. Additionally, the elevated CRP levels may reflect hyper-inflammation resulting from an uncontrolled immune response during moderate forms of COVID-19. Chest CT scans revealed that 89.4% of patients with moderate forms of COVID-19 had lung damage ranging from 10 to 50%. Ground glass opacities were the most commonly observed type of lesion. These findings were consistent with those reported by Islam N. et al, who found a similar prevalence of 87.9% [14]. Our findings revealed that moderate forms of COVID-19 associated with type 2 diabetes were characterized by an increased occurrence of parenchymal lesions in the form of ground-glass opacities. These lesions are likely caused by the direct damage inflicted by SARS-CoV-2, a virus that targets the lungs, on the pulmonary alveoli during the early stages of the disease [15].
Severe forms of COVID-19
In severe forms of COVID-19, our study found that acute respiratory distress was the most common clinical manifestation, affecting 50% of patients. This result is significantly higher compared to the study by Waechter C. et al, who reported only 20% of patients with severe forms of COVID-19, of which 5% were critical [7]. Respiratory distress syndrome is a common complication in severe forms of COVID-19. Our study results could be attributed to the destruction of lung parenchyma by SARS-CoV-2, as well as the uncontrolled hyper-inflammation and secondary hypercoagulability, which may lead to organ failure and result in respiratory distress syndrome [15,16]. Our research discovered that among patients with severe COVID-19 who also had type 2 diabetes, 77.8% exhibited lung involvement of over 50% as seen on chest scans without iodinated contrast product. The chest CT scans revealed widespread bilateral ground glass opacities, primarily in the posterior lung regions. This morphological analysis was crucial in diagnosing COVID-19 pneumonia in our population. The prevalence of ground glass opacities is believed to be caused by the "cytokine storm," a harmful mechanism causing accelerated damage to lung tissue [17,18]. It is important to note that not all patients with COVID-19 will experience severe disease, and the progression of the disease can vary greatly between individuals. Nevertheless, Figures 1 and 2 are valuable sources of information for healthcare professionals and researchers studying the disease in our region.
Other clinical and paraclinical manifestations of COVID-19
Our study, which included 65 patients with both forms of COVID-19 and diabetes, found that fever (56.9%) and tachycardia (23.1%) were common symptoms. These findings are consistent with a study by Waechter C. et al, where fatigue was the most common symptom reported in 63% of cases and fever in 55%." In addition to these symptoms, blood count abnormalities were also noted, affecting all three lineages. Hyperleukocytosis in 26.2% of patients, followed by anemia (18.5%), thrombocytopenia (13.8%) and lymphopenia (7.7%). These results differ from the findings of Waechter C. et al, who primarily reported leukopenia and lymphopenia. Our findings suggest a possible association between the elevated inflammation commonly observed in patients with type 2 diabetes and their susceptibility to COVID-19, possibly due to a compromised immune system response. This connection may be influenced by several factors, such as both short-term and long-term high blood glucose levels and the severity of COVID-19 symptoms, which can range from mild to severe [9,19-21]. However, further research is necessary in our region to fully understand the relationship between type 2 diabetes and COVID-19 and how to better manage and mitigate the associated health risks. Chest CT scans in both forms of COVID-19 revealed a common characteristic of sub-pleural consolidation in 80% of cases. This finding corresponds with the results reported by Zerah L. et al, who observed this phenomenon in 79% of cases [12].
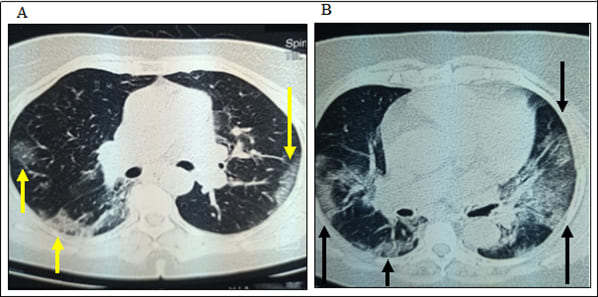
Figure 1: Distribution of lesions based on the degree of lung involvement in chest CT scans without iodinated contrast medium. Figure 1(A): Mild form of COVID-19, characterized by 35% lung damage (yellow arrows), displayed in an axial view with a lung window. Figure 1(B): Axial view of chest CT scan showing a severe form of COVID-19 with 50-60% of lung damage (black arrows). Images sourced from the COVID-HIA OBO Unit.
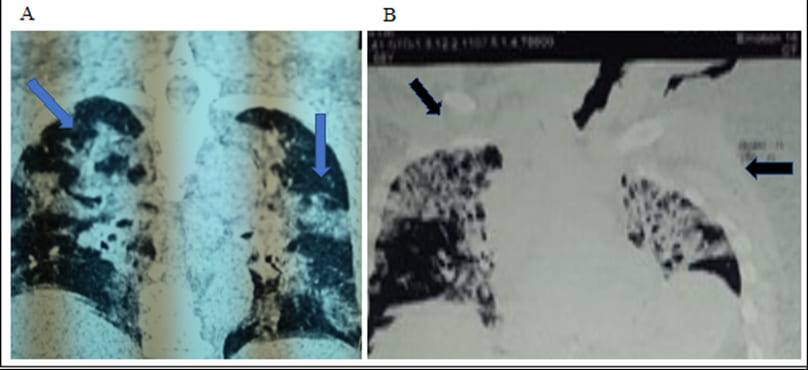
Figure 2: Chest CT scans in sagittal view of a severe form of COVID-19. Figure 2(A): illustrates 60-70% involvement of the lung tissue (blue arrows). Figure 2(B): displays a more advanced stage of the disease with over 80% of the lung parenchyma affected (black arrows). Images sourced from the COVID-Unit HIA OBO.
Biological indicators of Type 2 Diabetes Mellitus and COVID-19
Hyperglycaemia was the most frequently observed biological sign in COVID-19 patients, regardless of the clinical form of the disease, seen in 40% of cases. 30.8% of COVID-19 patients had HbA1c levels higher than 8%. This finding can be explained by the correlation between the severity of COVID-19 and the levels of inflammatory markers in patients with type 2 diabetes [19,22-25].
Acute complications of type 2 diabetes mellitus
Our study revealed that 18.5% of patients experienced an acute complication, with ketoacidosis being the most prevalent. This result is consistent with the findings of Djènèba M. et al, who reported a 19.2% occurrence of ketoacidosis in diabetes patients in Mali. In sub-Saharan Africa, ketoacidosis remains a significant challenge in the management of type 2 diabetes mellitus, and is often the result of late diagnosis and the exacerbating effects of infections such as COVID-19. To mitigate these risks, early detection of diabetes and provision of comprehensive care and support is crucial in preventing the onset of such acute complications [26,27].
Conclusion
This study highlighted the elevated risk faced by older adults and males in developing moderate to severe forms of COVID-19. The use of chest CT scans was deemed essential for accurate detection and assessment of lung lesions related to the disease. Furthermore, our findings indicated that diabetic ketoacidosis was the most frequently occurring acute complication among patients with type 2 diabetes, regardless of the manifestation of their COVID-19 infection.
Declaration of conflicting interests: The authors declared no conflicts of interest with respect to the research, authorship, and publication of this article.
Funding: The authors received no financial support for the research, authorship, and publication of this article.
References
- Gaye YE, Agbajogu C, El Oakley R (2021) COVID-19 on the Nile: Review on the Management and Outcomes of the COVID-19 Pandemic in the Arab Republic of Egypt from February to August 2020. Int J Environ Res Public Health. 18: 1588.
- Iroungou BA, Mangouka LG, Bivigou-Mboumba B, Moussavou-Boundzanga P, Obame-Nkoghe J, et al (2021) Demographic and Clinical Characteristics Associated With Severity, Clinical Outcomes, and Mortality of COVID-19 Infection in Gabon. JAMA Netw Open. 4: e2124190.
- Mveang Nzoghe A, Padzys GS, Maloupazoa Siawaya AC, Kandet Yattara M, Leboueny M, et al (2021) Dynamic and features of SARS-CoV-2 infection in Gabon. Sci Rep. 11: 9672.
- Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, et al (2020) Practical recommendations for the management of diabetes in patients with COVID-19. Lancet Diabetes Endocrinol. 8: 546-550.
- Collienne C, Castanares-Zapatero D, Apraxine M, Beauloye C, Capes A, et al (2020) Prise en charge aux soins intensifs des patients pour insuffisance respiratoire liée au COVID-19. Louvain Med. 139: 383-389.
- American Diabetes Association (2012) Diagnosis and classification of diabetes mellitus. Diabetes Care. 35: S64-71.
- Waechter C (2021) Manifestations cliniques et paracliniques de la COVID-19, diagnostic virologique. NPG Neurol - Psychiatr - Gériatrie. 21: 297-303.
- Donamou J, Touré A, Camara AY, Camara D, Camara ML, et al (2021) Predictive factors of mortality in patients with COVID-19 in Guinea: analysis of the first 140 cases admitted to intensive care unit. Pan Afr Med J. 38: 205.
- Yang X, Yu Y, Xu J, Shu H, Xia J, et al (2020) Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 8: 475-481.
- Endeshaw Y, Campbell K (2022) Advanced age, comorbidity and the risk of mortality in COVID-19 infection. J Natl Med Assoc. 114: 512-517.
- Medetalibeyoglu A, Senkal N, Kose M, Catma Y, Bilge Caparali E, et al (2020) Older Adults Hospitalized with Covid-19: Clinical Characteristics and Early Outcomes from a Single Center in Istanbul, Turkey. J Nutr Health Aging. 24: 928-937.
- Zerah L, Baudouin É, Pépin M, Mary M, Krypciak S, et al (2021) Clinical Characteristics and Outcomes of 821 Older Patients With SARS-Cov-2 Infection Admitted to Acute Care Geriatric Wards: A Multicenter Retrospective Cohort Study. J Gerontol Ser A. 76: e4-12.
- Nicolau J, Sanchís P, Dotres Fallat K, Romano A, Rodríguez I, et al (2022) Diabetes might not be a risk factor for worse prognosis among hospitalized patients due to COVID-19 in a Mediterranean area. Nutr Hosp. 39: 547-553.
- Islam N, Ebrahimzadeh S, Salameh JP, Kazi S, Fabiano N, et al (2021) Thoracic imaging tests for the diagnosis of COVID-19. Cochrane Database Syst Rev. 3: CD013639.
- Li X, Ma X (2020) Acute respiratory failure in COVID-19: is it “typical” ARDS? Crit Care. 24: 198.
- Ouédraogo AR, Bougma G, Baguiya A, Sawadogo A, Kaboré PR, et al (2021) [Factors associated with the occurrence of acute respiratory distress and death in patients with COVID-19 in Burkina Faso]. Rev Mal Respir. 38: 240-248.
- Tshienda FT, Tshikwela ML, Risasi JRM, Situakibanza HNT, Salem R, et al (2021) [Lesions on CT scan in patients hospitalized for coronavirus pneumonia during the first wave of the SARS-CoV-2 pandemic at the University Clinics in Kinshasa (DRC)]. Pan Afr Med J. 39: 230.
- Garnier M, Quesnel C, Constantin JM (2021) Atteintes pulmonaires liées à la COVID-19. Presse Médicale Form. 2: 14-24.
- Kosinski C, Zanchi A, Wojtusciszyn A (2020) Diabète et infection à COVID-19. Rev Médicale Suisse. 16: 939-943.
- Zhang JJ, Dong X, Cao YY, Yuan YD, Yang YB, et al (2020) Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 75: 1730-1741.
- Rahman A, Niloofa R, Jayarajah U, De Mel S, Abeysuriya V, et al (2021) Hematological Abnormalities in COVID-19: A Narrative Review. Am J Trop Med Hyg. 104: 1188-1201.
- Liu G, Zhang S, Hu H, Liu T, Huang J (2020) The role of neutrophil-lymphocyte ratio and lymphocyte–monocyte ratio in the prognosis of type 2 diabetics with COVID-19. Scott Med J. 65: 154-160.
- Mumu SJ, Saleh F, Ara F, Haque MR, Ali L (2014) Awareness regarding risk factors of type 2 diabetes among individuals attending a tertiary-care hospital in Bangladesh: a cross-sectional study. BMC Res Notes. 7: 599.
- Sultan A, Halimi S (2021) Relationship between type 2 diabetes and COVID-19: An update. Med Mal Metab [Internet].
- Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, et al (2019) Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 157: 107843.
- Lohourignon AL (2021) Screening and management of diabetes mellitus in Coted’Ivoire. Bull Acad Natl Med. 205: 566-573.
- Mauvais-Jarvis F, Sobngwi E, Porcher R, Riveline JP, Kevorkian JP, et al (2004) Ketosis-Prone Type 2 Diabetes in Patients of Sub-Saharan African Origin: Clinical Pathophysiology and Natural History of β-Cell Dysfunction and Insulin Resistance. Diabetes. 53: 645-653.

 research article
research article