Chemical Environment-Contaminating Substances in the Operating Room and Individual Exposure Levels
Miki Maruta1, Mutsuko Orita1, Yuki Matsuki2, Yutaka Tokuda3 Toshiyasu Suzuki4, Hideaki Matsuki5*
1Department of Nursing, Tokai
University Hospital, Japan
2Department of Future Prediction International
Health, Tokai University School of Medicine, Japan
3Department of Endocrine, Tokai University
School of Medicine, Japan
4Department of Anesthesiology, Tokai University
School of Medicine, Japan
5Department of Nursing, Tokai University School of Medicine, Japan
*Corresponding author: Hideaki Matsuki, Department of Nursing, Tokai University School of Medicine, Japan. Tel: +81-463902058; Email: hmatsuki@is.icc.u-tokai.ac.jp
Received Date: 11 October,
2018; Accepted Date: 02 November,
2018; Published Date: 14 November,
2018
Citation: Maruta M, Orita M, Matsuki Y, Tokuda Y, Suzuki T et al. (2018) Chemical Environment-Contaminating Substances in the Operating Room and Individual Exposure Levels. Arch Environ Sci Environ Toxicol: AESET-106. DOI: 10.29011/AESET-105 100006.
This research was based on a fact-finding examination of occupational exposure to formaldehyde among physicians and nurses engaged in surgery work, from a preventive perspective. More specifically, in operating rooms meeting current ventilation standards, measurements were taken of the concentration of Total Volatile Organic Compounds (TVOC), which are environment-contaminating substances in the air in these rooms, as well as the concentration of formaldehyde, dust, and odor. The examination found that the average TVOC concentration exceeded 400 micrograms per cubic meter, which is the provisional guideline indicated by the Japanese Ministry of Health, Labor and Welfare (MHLW), in nine of the 11 cases of operation (surgery) examined. The average formaldehyde concentration exceeded 80 ppb, which is the corresponding MHLW guideline, in six of the same 11 cases. Of the medical personnel involved in the operation cases, the average exposure concentration was highest among nurses indirectly assisting surgery (circulating nurses), followed in order by anesthesiologists, practitioners, and nurses directly assisting surgery (scrub nurses). These findings indicate that, even in operating rooms meeting the current ventilation standards, physicians and nurses engaged in surgery work are chronically exposed to toxic chemical substances in high concentrations. Such long-term exposure may be expected to increase risks of health impairment. In addition, volatile anesthetics are thought to be heavily involved in the formation of these chemical substances, and this points to the need for implementation of measures to counter contamination from surplus anesthetic gases and continuous monitoring of their levels. The research underscores the importance of implementing measures to lower exposure to environment-contaminating substances in the air for management of the work environment in operating rooms, and heightening awareness of the same among medical personnel.
Airborne environmental factors in operating rooms include many chemical substances, such as anesthetic gas; ethanol used for disinfection; Ethylene Oxide Gas (EOG) used for sterilizing instruments; volatile agents such as benzene and formalin used for fixing specimens; surgical smoke; Carbon Dioxide (CO2) used for endoscopic procedures; argon gas used in hemostasis and the like; and others [1]. Some of these chemical substances, such as EOG and formalin, contain carcinogens [2]. Handling of ethylene oxide, which is recognized as causing cancer in humans, has been strictly controlled since 2001, when the Industrial Safety and Health Act, Ordinance on Industrial Safety and Health, and Ordinance on Prevention of Hazards Due to Specified Chemical Substances were revised. In addition, based on revisions to the above laws in 2008, formaldehyde is considered a Class II specified chemical substance, and having its presence measured by occupational environment measurement experts once every six months is now mandatory [3].
Due to concern about the negative effects of anesthetic gas on the health of medical personnel, research on this issue has been conducted since the 1960s. A 1967 study by Vaisman focusing on anesthesiologists was the first to report that a high frequency of headaches, fatigue, and irritability was observed among anesthesiologists and, furthermore, that female anesthesiologists had a high miscarriage rate [4]. A large-scale 1974 study of around 50,000 operating room personnel and 24,000 other medical personnel conducted by the American Society of Anesthesiologists showed that women working in operating rooms had a high risk of miscarriage, cancer, liver disease, kidney disease, and birth defects in their children, while men working in operating rooms had a high risk of liver disease and birth defects in their children [5]. After considering countermeasures for operating room anesthetic gas contamination, the U.S. National Institute for Occupational Safety and Health (NIOSH) advised reducing the concentration of nitrous oxide (N2O) used in anesthetic gas to 25 ppm (0.025 ppb) or less [6]. In Japan as well, research on air quality contamination in operating rooms was conducted from the 1980s through the early 2000s. Based on this research, ventilation equipment has been improved and the use of surplus anesthetic gas scavenging systems has become more widespread. With advances in medicine, anesthesia methods and the anesthetics used have also changed, and it is now possible to use total intravenous anesthetics that involve no inhalation anesthetics or low-flow anesthetics that use small quantities of inhalation anesthetics. The frequency of use of nitrous oxide, once a standard anesthetic gas, has decreased, and volatile anesthetics such as Halothane and Isoflurane are being replaced with Sevoflurane. However, the manufacturing process for Sevoflurane, which is currently the most frequently used anesthetic, uses formaldehyde, hydrogen fluoride, and hexafluoro isopropanol [7], and degradation products during anesthesia that have been detected include chemical substances such as formaldehyde [8].
In addition, in recent years, attention has been called to the fact that there are many chemical substances in surgical smoke, which occurs when using electric scalpels. Currently, there is still a lot of uncertainty about the precise structural materials of surgical smoke [9], and there are no clear standards in Japan with respect to reducing exposure.
Currently, design and management principles for ventilation equipment in operating rooms are indicated in the Healthcare Engineering Association of Japan standard HEAS-02-2013 (Hospital Ventilation Equipment Guidelines), which incorporate the latest information from the U.S. Centers for Disease Controls and Prevention (CDC) and the like. In addition, standards relating to air quality have become higher based on the Act on Maintenance of Sanitation in Buildings. However, that does not mean that ongoing measurement is being carried out during operations, so the actual situation in terms of occupational exposure to chemical environment-contaminating substances among doctors and nurses engaged in surgery work is unclear. As a result, from a preventive standpoint, it is necessary to perform ongoing measurement of airborne chemical environment-contaminating substances in operating rooms, where physicians and nurses engaged in surgery work spend a lot of time and clarify their actual occupational exposure. Among chemical environment-contaminating substances, there is an especially high probability that formaldehyde will be produced during anesthesia, and since the ratio that this represents among Total Volatile Organic Compounds (TVOC) is also high, it would be preferable to measure this on its own. Such fact-finding examinations may serve as basic reference materials for developing measures to reduce chemical environment- contaminating substances in operating rooms.
The aim of this research is to measure the level of chemical environment-contaminating substances (TVOC, formaldehyde concentration, etc.) in the air of operating rooms that meet current ventilation standards, and from a preventive standpoint, clarify the actual level of occupational exposure to formaldehyde among physicians and nurses engaged in surgery work. The purpose is for the findings to serve as basic reference materials reducing and preventing exposure to such chemical environment-contaminating substances.
This study conducted environmental measurement in operating rooms in a hospital at “A” University and investigated the individual exposure levels of anesthesiologists, central operating room nurses, and breast/endocrine surgeons engaged in surgery work. The surgical procedures being undertaken were mastectomies, and the operating rooms were limited to rooms 11, 12, and 15 only, which had the same size (7 m×7 m×3 m = 147 m3), design, and ventilation equipment (amount of external air supplied to room: 750 m3/h; air circulation within room 4,680 m3/h). The conditions were the same as a normal procedure, with no restriction on entering and exiting the operating room during the surgery. As shown in (Table 1), the study covered 11 breast/endocrine surgeries conducted from July 2 to July 25, 2013.
Measurement of TVOC (Total Volatile Organic Compounds)
The TVOC gauge, formaldehyde gauge, digital dust gauge, temperature and humidity gauge, and the respective time measurement devices were set up in two locations: a position near the surgical field (1.5 m away, next to the operating table) and a position further away from the surgical field (about 3.5 m away, near the vent) (Figure 1).
For measuring TVOC, a FIGARO FTVR-01 TVOC monitor was used. This is a diffusion-type measurement device using a semi-conductor gas sensor with a measurement range of 0 to 10,000 μg/m3. In addition, it can perform continuous measurement at 2-second, 15-second, or 1-minute intervals and accumulate the results in a data logger inside the device. For this study, the measurement interval was set as 1 minute. TVOC measuring instrument which was used semiconductor sensor, therefore the indication level, it did not become the sum of individual price of real VOC. The calibration performed zero adjustment using the active carbon pipe of accessories. For formaldehyde measurement, a Shinyei Technologies FMM-MD formaldehyde multi-monitor was used. Using a colorimetric formaldehyde sensor, this device calculates formaldehyde concentration from the difference obtained when comparing the pre- and post-measurement results, based on photoelectric photometry.
Dust was measured using a Sibata Scientific Technology LD-3B digital dust gauge. This is a device that performs measurement based on a light scattering method, using a laser diode as the light source, and which can perform continuous measurement. Data was accumulated in the device using its logging function, then transferred to a computer with an LD-3B/3K2 software communication cable after measurement. For this study, the measurement interval was set as 1 minute. Temperature and humidity inside the operating room were measured using a T&D Illuminance-UV Recorder TR-74Ui. For this study, the measurement interval for temperature and humidity was set as 1 minute.
Practitioners, surgical assistants, nurses directly assisting surgery (scrub nurses), nurses indirectly assisting surgery (circulating nurses), and anesthesiologists were asked to wear a Supelco sampler (DSD-DNPH sampler: Diffusive Sampler for Determination with 2,4-dinitrophenylhydrazine) at their chest or waist during surgery. Those wearing the sampler were asked to indicate the times when they were in the operating room on a timesheet.
With the DSD-DNPH sampler, aldehydes and ketones that enter the diffusing filter due to molecular diffusion react with the 2,4-dinitrophenylhydrazine coated with silica gel, and it becomes a hydrazone derivative [10].
The Operation Is Performed as Shown Below
- The DSD-DNPH sampler was removed from its aluminum storage pouch, and the DNPH-impregnated silica gel was transferred to the side with the reservoir for elution by tapping the side of the sampler with the cap on the floor. Then, the storage container was removed. It was verified that the DNPH-impregnated silica gel had moved to the side with the elution tube, and if it had not, the step 1 procedure was repeated.
- The cap and diffusing filter were removed from the DSD-DNPH sampler, and the elution tube only was connected to the 57242-elution reservoir or a syringe barrel using a 28299-U adaptor, and the aldehyde/ketone-DNPH derivative was eluted with 5.0 mL of acetonitrile.
- Formaldehyde analysis of the aldehyde/ketone-DNPH derivative eluted with 5.0 mL of acetonitrile was performed using a Tosoh Corporation 8020-series HPLC (High Performance Liquid Chromatography).
- Injection amount: 20 μl,
- Moving bed: acetonitrile: deionized water = 6:4,
- Flow rate: 10 mL/min.,
- Analytical column: Waters symmetry C18 3.5μm, diameter: 4.6 m × length: 150 mm,
- Oven: 40。C,
- Detector: UV, 360 nm
Method of Calculating Individual Formaldehyde Exposure Level
The individual exposure concentration was calculated with the results of analyzing the aldehyde/ketone-DNPH derivative adsorbed by the DSD-DNPH sampler using HPLC.
The individual formaldehyde exposure level is shown as follows:
Individual exposure level concentration (ppb) = S (μg)a(μgppb/hr)×h(hr)
S (μg): collection amount, a (μg/ppb/hr): sampling rate,
h (hours): sampling time (hours)
Since the formaldehyde sampling rate, is 0.0053, the result is calculated based on [11,12]:
Individual exposure concentration level (ppb) = S (μg)0.0053(μgppb/hr)×sampling time(hr)
Surgical Smoke Formaldehyde Concentration Measurement
Surgical smoke that occurred during surgery was collected inside a suction bottle, and the concentration of formaldehyde contained in the smoke was measured. In terms of the collection method, surgical smoke that occurred in the surgical field was passed through a stainless-steel suction tube and suctioned into a Fit Fix suction container system with three Supelco DSD-DNPH samplers attached inside it. Three DSD-DNPH samplers were set inside the suction container system for each surgery case.
The method of extracting samples from the DSD-DNPH samplers, performing analysis using HPLC, and calculating the concentration inside the room was the same as for individual exposure level measurement. Based on the obtained data, key statistics such as average values and standard deviations were calculated. In addition, about comparison of average values between groups, we calculated the Welch t-test (significance probability = p<0.05) or Student’s t-test if unpaired and the Pearson correlation coefficient and tested the correlation coefficient (significance probability = P<0.05). The statistical software that was used was SPSS ver. 21.0 (serial no. 16071376) and HALWIN ver. 7 (serial no. 111908233).
When conducting the study, it was explained to the subjects that it was a research project on chemical environment-contaminating substances in operating rooms and individual exposure levels and that their participation was voluntary, and the survey was conducted after obtaining their consent. The research has been approved by the Tokai University School of Health Sciences Ethical Review Committee and Tokai University School of Medicine Ethical Review Committee.
For the surgeries performed in the 11 cases covered by this study, the shortest operating time was 1 hour 15 minutes and the longest was 6 hours 59 minutes. The shortest anesthesia time was 2 hours 6 minutes, while the longest was 8 hours (Table 1)
In addition, for all cases, a mixed gas consisting of air, oxygen, and Sevoflurane was used as an inhalation anesthetic, and in 7 of the 11 cases, formalin was used for specimen fixing in the operating room.
Measurement Results over Time for TVOC in Operating Room
For all 11 cases, the average values, standard deviations, maximum values, and minimum values for TVOC concentration at the two locations (next to the operating table, away from the operating table) from the time the patient entered the room until the time he or she left are shown in (Table 2). For all cases, the average value next to the operating table was higher than the average value away from the operating table. In addition, in 9 of the 11 cases, the average value next to the operating table exceeded the 2001 provisional guideline indicated by the Japanese Ministry of Health, Labour and Welfare (MHLW), which is 400 μg/m3 (the provisional targeted value of the general indoor environment), and the provisional guideline was also exceeded in 6 of 11 cases at the location away from the operating table. The maximum TVOC value next to the surgery table was 9,999 μg/m3 for the July 11 case, while away from the operating table, a maximum value of 8,020 μg/m3 was recorded for the July 25 case.
Changes over time in TVOC concentration on July 3 is shown in (Figure 2). During measurement, there were
two to four large peaks whose values exceeded 1,000 μg/m3. In addition, the figures show that while the measurement values away from the operating table were lower than the values next to the operating table, the wave form of changes over time was roughly the same. This was the same for all 11 cases.
Measurement Results over Time for Formaldehyde in Operating Room
The average values, standard deviations, maximum values, and minimum values for formaldehyde concentration at the two locations (next to the operating table, away from the operating table) from the time the patient entered the room until the time he or she left are shown in (Table 3). For all 11 cases, the average value next to the operating table was higher than the average value away from the operating table.
The management density by the work environmental measurement standard is 0.1ppm. In addition, the guidance level of the general indoor environment by the MHLW, is 80ppb, in 6 of the 11 cases, the average value next to the operating table exceeded the guideline level the maximum formaldehyde concentration value was 309 ppb next to the operating table, recorded for the July 10, July 11, and July 25 cases Changes over time in the formaldehyde concentration on July 3 and July 25 are shown in (Figure 3). During measurement, there were three large peaks whose values exceeded 80 ppb. In addition, the figures show that while the measurement values away from the operating table were lower than the values next to the operating table, the wave form of changes over time was roughly the same. This was the same for all 11 cases.
Measurement Results over Time for Dust Concentration in Operating Room
The average values, standard deviations, maximum values, and minimum values for dust concentration at the two locations (next to operating table, away from operating table) in the operating room for the 11 cases measured between July 2 and July 25 are shown in (Table 4). The average value results next to the operating table ranged from 0.97 μg/m3 to 3.91 μg/m3, while the maximum value was 24.8 μg/m3, which is extremely low compared to the operating room environment standard of 0.15 mg/m3 or less (150 μg/m3 or less) specified in the Act on Maintenance of Sanitation in Buildings.
Meanwhile, the average value results away from the operating table ranged from 1.17 μg/m3 to 2.84 μg/m3, while the maximum value was 24.8 μg/m3, which was lower than the operating room environment standard value indicated in the Act on Maintenance of Sanitation in Buildings.
As an example, changes over time in the dust concentration next to the operating table and away from the operating table on July 11 are shown in (Figure 4). Based on these results, no large peaks thrusting up from the wave form were observed during measurement, and no differences in dust concentration next to the operating table and away from the operating table were observed either. Similarly, no differences in dust concentration next to the operating table and away from the operating table were observed for the other measurement cases.
Measurement Results Over Time for Temperature and Humidity Inside Operating Room
In all cases, at both locations, the temperature was maintained at 25±2ºC, and no major changes were observed. No differences in temperature were observed between the two locations.
For all cases, the average humidity was maintained at 40% to 60%, and no significant fluctuations were observed. As with the temperature, no differences in humidity were observed between the two locations.
Individual Exposure Level Measurement Results
The measured individual formaldehyde exposure concentration statistics for practitioners, surgical assistants, nurses directly assisting surgery (scrub nurses), nurses indirectly assisting surgery (circulating nurses), and anesthesiologists are shown in (Table 5). Of the medical care personnel involved in the operations, the average exposure concentration was highest among nurses indirectly assisting surgery (circulating nurses), with an average value ± standard deviation of 94.0 ± 38.2 ppb, followed in order by anesthesiologists, practitioners, nurses directly assisting surgery (scrub nurses), and surgical assistants.
Average exposure concentration for nurses indirectly assisting surgery (circulating nurses), compared to exposure concentration for surgical assistants and nurses directly assisting surgery (scrub nurses) was significantly higher (p<0.05, Welch’s t-test). As well, the exposure concentration for anesthesiologists (87.9 ppb) was significantly higher than the exposure concentration for surgical assistants (p<0.05, Welch’s t-test). For all types of medical personnel, the maximum formaldehyde exposure concentration value exceeded the MHLW’s operating room concentration guideline value of 80 ppb (0.08 ppm).
Formaldehyde Concentrations Inside Suction Bottles (Table 5)
The concentration of formaldehyde that was collected and analyzed using the DSD-DNPH samplers attached inside the suction bottles had an average value ± standard deviation of 101.1 ± 58.6 ppb. This was significantly higher (P<0.05, Welch’s t-test) than the average concentration for practitioners, surgical assistants, and nurses directly assisting surgery (scrub nurses). As well, in 14 out of 33 samples, an exposure equal to or greater than the guideline value of 80 ppb (0.08 ppm) was observed.
Analysis of Correlation Between Individual Formaldehyde Exposure Concentrations of Medical Personnel and Formaldehyde Concentrations in Suction Bottles
We analyzed the correlation (Pearson’s correlation coefficient) between measured individual formaldehyde exposure concentration statistics for practitioners, surgical assistants, nurses directly assisting surgery (scrub nurses), nurses indirectly assisting surgery (circulating nurses), and anesthesiologists, the concentrations of formaldehyde inside the suction bottles, and the value next to the operating table and away from the operating table measured using the FMM-MD formaldehyde multi-monitor (Table 6). The results showed a significant correlation between practitioners and surgical assistants and nurses directly assisting surgery (scrub nurses) as well as between nurses directly assisting surgery (scrub nurses) and suction bottles 1 and 2 (p<0.01 or p<0.05).
DiscussionIn all 11 cases, the TVOC concentration and formaldehyde concentration average values from the time the patient entered the operating room until he or she left the operating room were both higher next to the operating table than they were away from the operating table. In 9 of the 11 cases, the average value next to the operating table exceeded the provisional targeted value of the general indoor environment of 400μg/m3 indicated by the MHLW, and this value was also exceeded in 6 of 11 cases at the location away from the operating table (Table 2). In addition, in 6 of the 11 cases, the average formaldehyde value next to the operating table exceeded 80ppb, which is the guidance level of the general indoor environment by the MHLW.
Many factors contribute to air quality inside operating rooms, but in the cases studied here, the anesthetic gas from pharmaceuticals and devices used during operations, surgical smoke, and formalin used for fixing specimens may be considered as air quality-contaminating factors.
The two to four large peaks observed in the measurement results over time for TVOC, formaldehyde, and odors coincided with the start of anesthesia, the start of reconstructive surgery following completion of the mastectomy, and the extubating of intubated tubes. In terms of the source of TVOC and formaldehyde, based on the wave form observed for the measurements over time and the timing of procedures during the operation, it may be assumed that anesthetic gas contributed significantly. In Arata, et al. [13], it is observed that there are so-called “hotspots” with high concentrations in proximity to anesthetic gas leakage points, but the average gas concentration level inside the operating room is determined by the amount of anesthetic gas that leaks during a given period and the amount of air that disperses and dilutes it. It has been reported that the amount of anesthetic gas that leaks varies depending on the anesthesia method, type of anesthetic apparatus, anesthetic gas concentration, flow rate, etc., while the amount of air is influenced by the air-conditioning method, the ventilation amount, the design of the operating room, the opening and closing of the door, the movement of people, etc. The diffusion of chemical substances is also affected by changes in temperature and humidity, but since the temperature and humidity were maintained at fixed levels, it may be assumed that they had no major effect on measurement of TVOC and formaldehyde exposure levels here.
In the 11 cases measured for this study, the only volatile anesthetic that was used was Sevoflurane. This is a volatile anesthetic that emits an odor and whose chemical structural formula is C4H3F7O. Formaldehyde, hydrogen fluoride, and hexafluoro isopropanol are used in the manufacturing process for Sevoflurane [7], and degradation products during anesthesia that have been detected include chemical substances such as formaldehyde [8]. There is concern about the effects of long-term exposure on health; there have been reports of it causing miscarriages, psychiatric symptoms, liver function impairment, and the like [14]. Moreover, formaldehyde is recognized as causing cancer in human beings and has been designated as a Class II specified chemical substance in the Ordinance on Prevention of Hazards Due to Specified Chemical Substances. About environmental exposure in operating rooms, in 1977 the National Institute for Occupational Safety and Health advised keeping halogenated inhalation anesthetic at 2 ppm (2,000 ppb) or less or 0.5 ppm (500 ppb) when used in combination with nitrous oxide [6]. Since this advice appeared, installation of anesthetic gas scavenging units has increased, and stricter safety standards have been introduced about air-conditioning. Various additional measures have been taken, such as reviewing anesthesia methods and conducting thorough inspections of the apparatus at the start of the procedure, which have made it possible to reduce contamination from surplus anesthetic gas in operating rooms. However, since continuous measurement is not actually being carried out during operations, at the current time, it remains unclear whether the NIOSH and Japanese Society of Anesthesiologists’ guidelines are being met while surgical procedures are being performed.
Surgical smoke occurs after the start of surgery, but no pronounced peaks in either TVOC or formaldehyde were observed after the start of surgery. Based on this, the surgical smoke that was measured at the two points in the operating room may be considered to have little effect.
About formalin used for fixing specimens, sealed containers of formalin were brought into the operating room in all cases, but they were only opened and used inside the operating room in 7 cases. Differences in the changes over time in TVOC and formaldehyde were observed between the 7 cases where formalin was used and the 4 cases where it was not used. In the cases where formalin was used, since formalin containers were often opened when processing specimens in the operating room after completing surgery, peaks with high concentrations of TVOC and formaldehyde appeared after the completion of surgery. One of the peaks observed in Figure 3, occur during the time period between the completion of the mastectomy operation and the start of reconstructive surgery. During this time period, the surgeon was often processing specimens in the operating room, so one would expect the effect of formalin for fixing specimens to be significant.
Based on the present study, TVOC and formaldehyde were detected as air quality-contaminating substances inside the operating room, and it was clear that physicians and nurses engaged in surgical work were exposed to chemical substances on a chronic basis. In addition, results were obtained that strongly suggest that leakage of surplus anesthetic gas and the effects of formalin used to fix samples are causes of air quality contamination. At the hospital where the study was conducted, physicians, nurses, and the operating room’s dedicated clinical engineer verify that the anesthetic gas scavenging system has started up and that the anesthetic apparatus is functioning properly by inspecting it before starting the procedure, so it is difficult to imagine that anesthetic gas leaks occurred due to equipment malfunctions, and the current anesthetic gas leak countermeasures may be considered to prevent anesthetic procedure-related leaks as much as possible. From the perspective of occupational safety, continuous monitoring during surgery may be considered necessary. About formalin used for fixing samples, it has been stipulated that the procedure should be performed in a well-ventilated location, but countermeasures such as choosing a location that will avoid exposing other personnel to formalin as much as possible and making it mandatory for the person performing the procedure to wear protective gear are necessary.
Meanwhile, with regard to dust concentration at the two locations (next to the operating table, away from the operating table) in the 11 cases, the average value, standard deviation, maximum value, and minimum value results show that the average value results next to the operating table ranged from 0.97 μg/m3 to 3.91 μg/m3, with a maximum value of 24.8 μg/m3, which is extremely low compared to the standard value of 0.15 mg/m3 or less (150 μg/m3 or less) specified in the Act on Maintenance of Sanitation in Buildings and Healthcare Engineering Association of Japan standard HEAS-02-2013 (“Hospital Ventilation Equipment Guidelines).
The operating rooms at “A” University hospital are advanced facilities which control airborne dust inside the room via the air pressure and airflow from the ceiling with an air-conditioning system that uses high-performance filters. The measurements over time conducted in this study made it clear that the dust concentration inside the operating rooms was well within the required standards and that the movement of people in the rooms had little effect on dust concentrations.
Individual Exposure Levels
Formaldehyde is a colorless, water-soluble gas which is an important chemical substance used in production of synthetic urea- and phenol-formaldehyde resins. Typically, these resins are employed as adhesives when producing particle board, fiber board, plyboard, and so forth. Concentrated urea-formaldehyde is used in production processes for coatings, paper, etc., as well as in foam insulation.
Tearing and irritation of the eyes and upper respiratory passages due to formaldehyde can be felt at concentrations ranging from 0.1 to 5 ppm (100 to 5,000 ppb). The odor of formaldehyde starts to be noticeable from 1 ppm (1,000 ppb), but depending on the person, it may be detected even starting from 0.05 ppm (50 ppb). At concentrations of 10 to 20 ppm (10,000 to 20,000 ppb), exposed individuals will begin to experience coughing and chest constriction, heavy-headedness, and an increased heart rate. These symptoms may occur at 5 ppm (5,000 ppb) or less in highly sensitive individuals, while it has been reported that exposure to concentrations of 0.25 to 5 ppm (25 to 5,000 ppb) has caused severe asthma attacks in bronchial asthma patients [15], T.D., 1984). Exposure to 50 to 100 ppm (50,000 to 100,000 ppb) or more has been said to trigger pulmonary edema or pulmonary alveolitis, while exposure to 100 ppm (100,000 ppb) or more has been known to be fatal [16]. In addition, formaldehyde has been observed to be cancerous in animal experiments conducted at the U.S. Chemical Industry Institute of Toxicology [17]. In terms of industrial safety, guidelines have indicated that the permissible concentration of formaldehyde is 0.1 ppm (100 ppb) in work environments and 0.08 ppm (80 ppb) in general indoor environments.
The results of individual exposure level measurements in this research showed that, among the medical professionals engaged in surgeries, exposure to formaldehyde was highest for nurses indirectly assisting surgery (circulating nurses), with an average concentration ± standard deviation of 94.0 ± 38.2 ppb (0.094 ± 0.038 ppm), followed in order by anesthesiologists, practitioners, nurses directly assisting surgery (scrub nurses), and surgical assistants.
Compared to the exposure concentration for surgical assistants and nurses directly assisting surgery (scrub nurses), the average exposure concentration for nurses indirectly assisting surgery (circulating nurses) was significantly higher (P<0.05, Welch’s t-test). As well, the exposure concentration for anesthesiologists (88 ppb) was significantly higher than the exposure concentration for surgical assistants (P<0.05, Welch’s t-test). Possible reasons why the exposure concentrations were higher for nurses indirectly assisting surgery (circulating nurses) and anesthesiologists compared to the other study subjects are the fact that anesthetic gas may have been a key element in formaldehyde incidence in this study and, in addition, the fact that, during surgery, it is the anesthesiologist who performs the anesthetic procedure near the patient’s head, including tasks such as anesthesia induction and extubation. In the case of circulating nurses, the reason may be that they play a role in assisting the anesthesiologist with the aesthesia process and are the person who works closest to the anesthesiologist and patient during anesthesia induction and extubation.
For all of the medical personnel, the maximum formaldehyde exposure concentration exceeded the MHLW’s guideline value for operating concentration levels, which is 80 ppb (0.08 ppm). Given this, it is clear that medical personnel engaged in surgery work are being exposed to formaldehyde on a chronic basis.
Formaldehyde in Surgical Smoke
In recent years, attention has been focused on the fact that surgical smoke contains many chemical substances. Surgical apparatus such as electrical scalpels, lasers, and ultrasonic scalpels destroy tissue by applying energy to it. At that time, cells are subject to abrupt heating, causing moisture in cells to vaporize, expand, and rupture, particulates containing cell contents to form, and carbides containing hazardous substances to form at the same time. The average particle diameter of surgical smoke is 0.35 to 6.5 μm for electrical scalpels [18], which is significantly smaller than the particle size (>5 μm) that surgical masks are effectively able to capture. This means that it is easy for these particles to be inhaled by medical personnel and deposited in their respiratory tract or lungs [1]. There are reports confirming the presence of acetaldehyde, acrolein, benzene, formaldehyde, toluene, xylene, and so forth in surgical smoke, but there are still many uncertainties in terms of the precise structural material [9]. Furthermore, these chemical substances have carcinogenetic properties, with the carcinogenicity of smoke produced by 1 g of cauterized tissue being equivalent to 3 cigarettes in the case of a laser or 6 cigarettes in the case of an electrical scalpel [19].
In this study, surgical smoke produced using electrical scalpels was collected by means of DSD-DNPH samplers attached inside suction bottles and analyzed. The average formaldehyde concentration value ± standard deviation was 101.1 ± 58.6 ppb (Table 5), and in 14 out of 33 samples, an exposure equal to or greater than the guideline value of 80 ppb (0.08 ppm) was observed. This was significantly higher (p<0.05, Welch’s t-test) than the average concentration for practitioners, surgical assistants, and nurses directly assisting surgery (scrub nurses). Surgical smoke is one of the key factors in individual exposure to formaldehyde among practitioners, surgical assistants, and nurses directly assisting surgery (scrub nurses), so if they continue to be exposed to it without it being suctioned, their individual formaldehyde exposure level may increase further. Moreover, long-term exposure could lead to impaired health.
The operating rooms covered by this study were not equipped with suction devices specifically for surgical smoke. However, in view of the toxicity of the fumes produced when living tissue is cauterized, the Japanese Association for Operative Medicine recommends forced ventilation of smoke produced during surgery with specialized surgical smoke suction devices, so that patients and medical staff do not inhale it [20]. While suction devices for blood are of some use in suctioning surgical smoke, the suction rate is low, and they cannot eliminate smoke in sufficient quantities. Currently, installation of dedicated suction devices is not mandatory, and, as is the case for anesthetic gas leaks, monitoring is not performed, so physicians and nurses may have little awareness of the health risks due to exposure to surgical smoke.
Given these findings, it is necessary for physicians and nurses engaged in surgery work to recognize the reality that they are constantly being exposed to TVOC and formaldehyde and to raise awareness so that the risk factors will be reduced as much as possible. It is also necessary for anesthesiologists to consider procedures for preventing anesthetic gas leaks. And in terms of managing workers’ health, it would be preferable to give special consideration to pregnant or nursing women and people at high risk of health impairment, such as transferring them to a location where there is a low probability of exposure to chemical environment-contaminating substances.
The authors declare that they have no conflict of interest.
AcknowledgmentsWith regard to the conducting of this research, we would like to express our heartfelt gratitude to all the breast and endocrine surgery medical staff, anesthesiology medical staff, and central operating room nurses at the hospital affiliated with “A” University’s school of medicine who collaborated on the study.
Figure
1: Position of The Measuring in The
Operating Room.
Figure 2: Change with time of TVOC concentration (case of July 3, 2013)
---- Next to operation table ----- Away from operation table.
Figure 3: Change with time of formaldehyde concentration (case of July 25,
2013) ---- Next to operation table ----Away from operation table.
Figure 4: Change with time of Dust concentration (case of July 11, 2013)
---- Next to operation table ----Away from operation table.
|
Operation day |
Operation time |
Anesthesia time |
|
2-July |
1hrs.35min. |
2hr.10min. |
|
3-July |
6hrs. 35min. |
8 hrs. |
|
8-July |
1 hrs. 46 min. |
2 hrs. 38 min. |
|
9-July |
1 hrs.48 min. |
2 hrs.30 min. |
|
10-July |
3 hrs.25 min. |
4 hrs.22 min. |
|
11-July |
6 hrs.29 min. |
7 hrs.11 min. |
|
17-July |
1 hrs.28 min. |
2 hrs.6 min. |
|
18-July |
1 hrs.15 min. |
2 hrs.10 min. |
|
19-July |
3 hrs.55 min. |
4 hrs.48 min. |
|
24-July |
3 hrs.10 min. |
3 hrs.56 min. |
|
25-July |
6 hrs. |
7 hrs.39 min. |
Table1: An Operation day and operative time.
|
Operation day |
Next to the operating table(µg/m3) |
Away from the Operating table(µg/m3) |
||||||
|
Mean |
± S.D. |
Max. |
Min. |
Mean |
±S.D. |
Max. |
Min. |
|
|
02-July |
1975 |
± 1806 |
7220 |
198 |
1970 |
± 1823 |
7836 |
144 |
|
03-July |
1699 |
± 1396 |
7070 |
401 |
1076 |
± 1313 |
5638 |
0 |
|
08-July |
409 |
± 209 |
1185 |
34 |
115 |
± 140 |
590 |
0 |
|
09-July |
427 |
± 511 |
3875 |
61 |
148 |
± 311 |
1457 |
0 |
|
10-July |
995 |
± 983 |
4208 |
0 |
761 |
± 915 |
3888 |
0 |
|
11-July |
1174 |
± 1260 |
9999 |
175 |
589 |
± 1191 |
7916 |
0 |
|
17-July |
392 |
± 434 |
1882 |
0 |
225 |
± 317 |
899 |
0 |
|
18-July |
392 |
± 414 |
3734 |
0 |
342 |
± 345 |
1462 |
0 |
|
19-July |
412 |
± 720 |
5429 |
0 |
300 |
± 665 |
4352 |
0 |
|
24-July |
628 |
± 562 |
2348 |
0 |
611 |
± 462 |
2107 |
122 |
|
25-July |
1156 |
± 854 |
5086 |
428 |
963 |
± 1687 |
8020 |
0 |
Table 2: Measurement Result of TVOC in Operating Room.
|
Operation day |
Next to the Operating table(ppb) |
Away from the Operating table (ppb) |
||||||
|
Mean |
±S.D. |
Max. |
Min. |
Mean |
±S.D. |
Max. |
Min. |
|
|
2-July |
128 |
±98 |
280 |
30 |
28 |
±25 |
61 |
0 |
|
3-July |
98 |
±94 |
260 |
20 |
50 |
±50 |
198 |
12 |
|
8-July |
47 |
±17 |
69 |
24 |
32 |
±9 |
52 |
26 |
|
9-July |
102 |
±76 |
248 |
40 |
51 |
±68 |
152 |
0 |
|
10-July |
167 |
±102 |
309 |
25 |
45 |
±54 |
164 |
0 |
|
11-July |
87 |
±100 |
309 |
11 |
22 |
±19 |
61 |
0 |
|
17-July |
23 |
±21 |
62 |
0 |
9 |
±8 |
21 |
0 |
|
18-July |
67 |
±51 |
146 |
12 |
29 |
±18 |
61 |
11 |
|
19-July |
44 |
±5 |
49 |
35 |
27 |
±7 |
38 |
17 |
|
24-July |
62 |
±29 |
131 |
31 |
32 |
±20 |
61 |
12 |
|
25-July |
95 |
±86 |
309 |
18 |
55 |
±41 |
164 |
12 |
Table 3: Measurement Results of Formaldehyde in operating room.
|
Operation day |
Next to the operating table (µg/m3) |
Away from the operating table (µg/m3) |
||||||
|
Mean |
± S. D |
Max. |
Min. |
Mean |
± S. D |
Max. |
Min. |
|
|
02-July |
1.7 |
±1.4 |
7.2 |
0 |
1.6 |
±1.3 |
6.4 |
0 |
|
03-July |
2.5 |
±2.7 |
18.4 |
0 |
2.1 |
±2.2 |
20 |
0 |
|
08-July |
2.2 |
±2.2 |
13.6 |
0 |
1.7 |
± 1.5 |
8.8 |
0 |
|
09-July |
1.4 |
±1.3 |
5.6 |
0 |
1.4 |
±1.6 |
8 |
0 |
|
10-July |
2 |
±1.8 |
12 |
0 |
2.1 |
±1.9 |
12.8 |
0 |
|
11-July |
2.8 |
±2.9 |
22.4 |
0 |
2.1 |
±2.0 |
12.8 |
0 |
|
17-July |
1 |
±0.9 |
6.4 |
0 |
1.3 |
±1.4 |
7.2 |
0 |
|
18-July |
1.5 |
±1.0 |
6.4 |
0 |
1.8 |
±1.2 |
5.6 |
0 |
|
19-July |
3.9 |
± 4.4 |
24.8 |
0 |
2.8 |
±2.8 |
20.8 |
0 |
|
24-July |
1.8 |
±1.8 |
10.4 |
0 |
1.9 |
±2.0 |
10.4 |
0 |
|
25-July |
1.8 |
±2.4 |
15.2 |
0 |
1.1 |
±1.4 |
17.6 |
0 |
Table: 4 Measurement Result of Dust in operating Room (µg/m3).
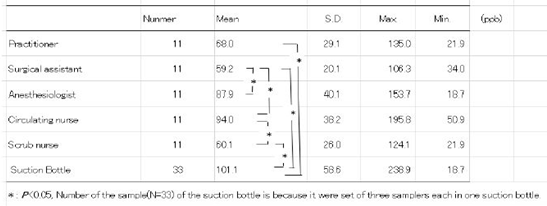
Table 5: Individual Exposure level of formaldehyde Lenel in medical Staff and in suction bottele.
|
|
practitioner |
surgical assistant |
anesthesiologist |
circulating nurse |
scrub nurse |
1 |
2 |
3 |
|
practitioner |
1 |
0.720* |
0.034 |
-0.1 |
0.846** |
0.295 |
0.554 |
0.351 |
|
surgical assistant |
|
1 |
0.164 |
0.016 |
0.415 |
-0.094 |
-0.095 |
-0.0202 |
|
anesthesiologist |
|
|
1 |
0.532 |
-0.073 |
0.03 |
0.011 |
-0.047 |
|
circulating nurse |
|
|
|
1 |
-0.006 |
0.031 |
-0.191 |
-0.063 |
|
scrub nurse |
|
|
|
|
1 |
0.643* |
0.643* |
0.587 |
|
Suction bottle 1 |
|
|
|
|
|
1 |
0.743** |
0.831** |
|
Suction bottle 2 |
|
|
|
|
|
|
1 |
0.924 |
|
Suction bottle 3 |
|
|
|
|
|
|
|
1 |
Table 6: correlation coefficient between individual formaldehyde exposure level of medical staff and
- Kai T (2009) Anesthesiologists and the operating room environment-from the view of air environment Masui. 58: S225-S223.
- Japan Society for Occupational Health (2013) Recommendation of occupational exposure limits (2013- 2014). Sangyo Eiseigaku Zasshi 55 : 182-208.
- Ministry of Health, Labour and Welfare (2008) Revision such as specified chemical substance disorder Ordinance on Prevention of December 2007. (in Japanese) Ministry of Health, Labour and Welfare Tokyo. (2014.1.20 search).
- Vaisman AI (1967) Working conditions in the operating room and their effect on the health of anesthetists. Eksp Khir Anesteziol 12: 44-49.
- American Society of Anesthesiologists (1974) Occupational disease among operating room personnel A national study. Report of an ad hoc committee on the effect of trace anesthetics on the health of operating room personnel, American society of anesthesiologists. Anesthesiology 41: 321-340.
- National Institute for Occupational Safety and Health (NIOSH) (1977) Criteria for a recommended standard Occupational exposure to waste anesthetic gases and vapors. DHEW (NIOSH) 77-140 U.S. Department of Health, Education, and Welfare, Washington, DC 194PP.
- Overton G (2011) IR countermeasure aim for safer flights. Laser Focus World 47: 35-43.
- Weida MJ, Buerki P, Takeuchi E, Day T (2010) External-cavity QCLs broaden capabilities for molecular detection. Laser Focus World 46: 58-62.
- Nagoya T, Ishikawa A (2002) The chemical compound of surge Cal smoke developing for laser scalpel utilization time. Sangyo Eiseigaku Zasshi 44.
- Uchiyama S, Hasegawa S (1999) A reactive and sensitive diffusion sampler for the determination of aldehydes and ketones in ambient air. Atmos Environ 33: 1999-2005.
- Yanagisawa Y, Noguchi M (2010) Carbonyl compound. Indoor Environment 13: 47-54.
- Uchiyama S, Aoyagi S, Ando M (2004) Evaluation of a diffusive sampler for measurement of carbonyl compounds in air. Atoms Environ 38: 6319-6326.
- Arata, Shimizu, Kawakami, Tomita T, Mitsuoka T, et al. (1980) Contamination of the operating room by waste anesthetic gases. Okayama Med Assoc 92: 115-123 (in Japanese).
- Kawatani Y, Kuwahara E, Shintani T, Sugawara M, Takita A, et al. (2006) Anesthetic gas level during exhalation of operating room staff. 27: 362-364.
- Sterling TD (1984) Economics and politics in the assessment of causes of building illness the NAS/NRC report on indoor pollutants. Int J Health Serv 14: 43-53.
- Feron VJ, Til HP, de Vrijer F, Woutersen RA, Cassee FR et al. (1991) Aldehydes occurrence, carcinogenic potencial, mechanism of action and risk assessment. Mutat Res 259: 363-385.
- Kerns WD, Pavcov KL, Donofrio DJ, Gralla EJ, Swenberg JA (1983) Carcinogenicity of formaldehyde in rats and mice after long-term inhalation exposure. Cancer Res 43: 4382-4392.
- Ulmer BC (2008) The hazards of surgical smoke. AORN J 87: 721-738.
- Alp E, Bijl D, Bleichrodt RP, Hansson B,Voss A (2006) Surgical smoke and infection control. J Hosp Infect 62: 1-5.
- Japanese Association for operative Medicine (2013) An operation medical practice guideline, revised edition, 34: S105-S107.

 research article
research article