Oritavancin for the Treatment of Infective Endocarditis due to Gram-positive Organism
David
A. Terrero Salcedo*, Rima
El-Herte, Michele Granada
Department of Internal Medicine, Mercy Medical Center, Des Moines, IA, USA
*Corresponding author: David A. Terrero Salcedo, Department of Internal Medicine, Mercy Medical Center, Des Moines, IA 50314-2610, USA. Tel: +13478131610; +15152474240; Fax: +15152474239; Email: daveterrero@gmail.com
Received Date: 06August, 2018; Accepted Date: 22 August, 2018; Published Date: 30 August, 2018
Citation: Terrero Salcedo DA, El-Herte R, Granada M (2018) Oritavancin for the Treatment of Infective Endocarditis due to Gram-positive Organism. Ann Case Rep: ACRT-202. DOI: 10.29011/2574-7754/100102
1. Introduction
The new lipoglycopeptides were developed in an effort to overcome
the increase prevalence of Methicillin-Resistant Staphylococcus aureus (MRSA) and other Gram-positive organisms. All three members
of the group (Dalbavancin, Telavancin and Oritavancin) have proven to treat
serious Gram-positive infection in animals, such as endocarditis, bacteremia
and pneumonia [1-4]. Observational studies have
also shown successful treatment of osteomyelitis and joint infection in humans
[5,6]. Nace and Lorber documented what
they believed was the first case of successfully treated MRSA endocarditis in
an intravenous drug user (IVDU) patient with Telavancin [7]. Recently, Tobudic S. et al. demonstrated a 92.6%
success rate treating infective endocarditis (IE) with Dalbavancin [8]. At present, these drugs are only approved by the
Food and Drug Administration (FDA) to treat acute bacterial skin infections [9].
An important property of these agents is their lipid side chains, which anchors the molecule to the cell membrane and concentrates the drug at its site of action [10]. Both Dalbavancin and Oritavancin have a half-life of 250 and 340 hours respectively, as opposed to Telavancin, with a half-life of 6-8 hours [3]. Oritavancin is unique in that it is not metabolized and has shown to dissipate membrane potential, carrying clinical implications in its activity against slowly growing organisms and biofilms [11,12].
Patients who inject drugs and require long term intravenous therapy pose a major challenge in clinical practice. It is not preferable to discharge these patients with central venous catheters for well-known reasons. Hence, the practice varies between having patients coming for daily infusion or treatment in the inpatient setting. The availability of a very specific anti-staphylococcal agent with a long half-life requiring injection every 1-2 weeks seems very practical. However, there are no randomized trials that have assessed the efficacy of Oritavancin or Dalbavancin in treatment of blood stream and other endovascular or deep-seated infections.
Herein, we provide a case series of five patients with selected Gram-positive bacteremia and endocarditis treated with Oritavancin with description of the subsequent outcomes.
2. Methods
This is a case series of five patients who inject drugs (PWID) with a diagnosis of infective endocarditis due to Gram-positive organisms, that were admitted to our institution between December 2017 and February 2018.
Patients were initially started on empiric antimicrobials and
rapidly switched to standard of care treatment. Blood cultures were incubated
in BacT/Alert 3D system by Biomerieux. Gram stain was performed when the system
signaled a growth and later ran through a Verigene SP Nanosphere Automated
System version 2.0 by Luminex. This aided identifying species and subspecies as
well as the presence of the mecA gene to determine Methicillin resistant
organisms. Susceptibility was performed using a Microscan Walkaway 96 Plus by
Siemens. Patients were given Oritavancin according to the discrimination of the
infectious diseases consultant. The treatment duration was according to what is
recommended by the IDSA recommendation for infective endocarditis. Patients
were scheduled to receive 1200 milligrams of Oritavancin for three hours weekly
at our infusion center and be evaluated by an infectious disease physician.
Weekly surveillance labs were obtained consisting of complete blood count,
basic metabolic panel and ALT. Within one week after the end of the treatment,
blood cultures were again obtained for surveillance. Once identified,
institution review board approval was obtained.
3.
Report of Cases
3.1. Case 1
A 44-year-old man was seen in our emergency department with initial complaint of fever, malaise and chills, He has end-stage renal disease and prior use of intravenous drugs. Blood culture obtained at presentation grew MSSA. After having received empirical therapy, treatment was switched to Cefazolin. A Transesophageal Echocardiogram (TEE) showed a vegetation and abscess on the Mitral Valve (MV). Valve replacement was performed after 2 weeks of treatment. Pathology and culture were negative for inflammation and growth. While inpatient, he received Cefazolin. At discharge, due to the suspected history of intravenous drug abuse, the infectious disease consultant recommended the use of Oritavancin, with the first dose being administered prior to discharge and subsequent doses weekly until total of 4 doses. Blood cultures reported to be negative 30 days after treatment. A TEE performed a month after his last dose did not show evidence of abscess or vegetation.
3.2. Case 2
A 30-year-old PWID man was seen in our emergency room for a three-day history of chest pain, myalgia and shortness of breath. Initial work up showed multiple pulmonary septic emboli with possible cavitation. Later, the blood cultures grew MRSA. His Transthoracic Echocardiogram (TTE) showed a Tricuspid Valve (TV) vegetation. Empirical treatment was simplified to Vancomycin. On day 4 of admission, patient developed a rash which was suspected to be due to Vancomycin, and therapy was switched to Ceftaroline. Due to the active illicit drug injection, the infectious disease consultant recommended weekly treatment with Oritavancin to complete 6 weeks duration as outpatient. He received one dose prior to discharge and never returned for his remaining doses. He was evaluated 8 weeks later in our emergency department for intravenous opiate overdose. At that time, there were no reported complaints.
3.3. Case 3
A 24-year-old woman with active illicit drug use was hospitalized
for chest pain and fever. She has a history of treated Hepatitis C. Initial
evaluation showed multifocal pulmonary infiltrates. Blood cultures collected at
presentation grew MRSA. A TEE showed a tiny flair leaflet fragment in the MV
suggesting a vegetation. The patient was initially on treatment with vancomycin.
Due to active drug use, the infectious disease consultant chose to treat her
with daily injection of daptomycin at the OPAT (Outpatient Parenteral
Antibiotic Therapy) center for six weeks. However due to social hindrances, the
patient was admitted for inpatient treatment with vancomycin. The week before
the end of her treatment, the patient manipulated her venous access and was
given one dose of Oritavancin to conclude her treatment. The same day she
received Oritavancin, she developed hypotension, fevers, rash and eosinophilia.
She was treated symptomatically. Follow up after 30 days of treatment did not
show evidence of clinical relapse and repeated blood cultures were negative.
3.4. Case 4
A 36-year-old man actively injecting illicit drugs was admitted for multiple abscesses in both arms. Prior to his visit at another medical center, the patient had drainage of the abscesses and was given trimethoprim-sulfamethoxazole. After empirical treatment with vancomycin, treatment was switched to cefazolin as his abscesses cultures grew Streptococcus pyogenes (Group A) and Beta-hemolytic group F Streptococcus. Blood cultures were negative. As the patient was found to have a systolic murmur, a TEE was performed showing a sessile vegetation in one of the leaflets of the TV. Since the patient had already been on antibiotics prior to this admission, negative blood culture samples were suspected to be false negative. Patient was treated for infective native TV endocarditis. Given his social history, substance risk behavior and medication interaction that preclude the use of other oral options, the infectious diseases consultant recommended to treat the patient with Oritavancin. A first dose was administered in the hospital prior to discharge. The patient successfully completed the outpatient treatment for total of four doses. Two weeks after the end of the treatment a repeated TEE did not show any vegetations.
3.5. Case 5
A 32- year-old woman with active illicit intravenous drug use was admitted with a 3-day course of pleuritic sharp right sided chest pain, fever, chills and dysuria. Further work up showed the presence of right lung lower lobe infiltrates, septic emboli of the lungs and a TV vegetation and perforation by TEE. Her blood cultures obtained at presentation grew MSSA. Her initial antimicrobial therapy was simplified to Cefazolin. This was switched to vancomycin due to skin rash and eosinophilia. She later underwent decortication of the right lung due to developing empyema. Once ready for discharge, due to the active illicit drug injection, the infectious diseases consultant recommended the use of oritavancin as weekly infusions for 6 weeks. She received her first dose prior to discharge and never returned for follow up nor for Oritavancin infusion. She was lost to follow-up. (Table 1)
*: Cure achieved by negative blood culture and clinical resolution.
**: First antimicrobial agent represents the initial choice which
was later switched to a second agent.
Abbreviations: M: Male, F: Female, MV: Mitral Valve, TV: Tricuspid Valve, MSSA: Methicillin-Sensitive Staphylococcus aureus, MRSA: Methicillin-Resistant Staphylococcus aureus, GAS: Group A Streptococcus, GFS: Group F Streptococcus, NR: Not Reported, ND: Not Determined.
4.
Discussion
Our patients who completed the full treatment with Oritavancin did not have relapse on followed up. Only one patient had an allergic reaction that was managed without negative consequences. It was unclear for what reason the other two patients did not pursue the treatment. No metabolic derangements were observed while on treatment.
Our manuscript is not the first to report an off -label use of Oritavancin to treat an infection for which is not approved for as last resort use. Johnson et al. reported treating a patient with recurrent vancomycin resistant Enterococcus faecium (VRE) bacteremia due to infective endocarditis [13]. Their patient had a VRE with a significant resistance profile who did not tolerate other lines of treatment. Their patient received a twice weekly 1200 mg infusion for 7 weeks after source control with remission of his infection. Stewart et al. published a report of 10 patients with various Gram-positive invasive infections treated with Oritavancin, including MSSA bacteremia, MRSA bursitis, Group B streptococcal bacteremia with native TV infective endocarditis, Coagulase-negative staphylococcal bacteremia, MSSA deep tissue infection, and enterococcal bacteremia. Oritavancin was well tolerated, and 7/10 patients were successfully treated [14]. Two case reports have now been recently generated elaborating on the success of treatment of MRSA native vertebral osteomyelitis and tibial shaft osteomyelitis [15].
Animal models of MRSA endocarditis, VRE endocarditis, VRE central
venous catheter infection, pneumococcal meningitis and in a human model of Clostridium difficile infection showed successful
results in treatment with Oritavancin [16-20].
Oritavancin seemed to be a convenient option for patients who have contraindication for long term catheter insertion for intravenous treatment such as lack of vascular access, recurrent thrombosis and intravenous illicit drug use as it needs to be given only once weekly. Other reasons for its use were failure of other standard of treatments. Oritavancin has a relatively safe profile aside from increase in transaminases, interference with coagulation studies and possible osteomyelitis. In case when an allergic reaction occurs, Oritavancin is not dialyzable. In our series, only one patient suffered an allergic reaction which was treated with oral prednisone, with complete resolution.
There are no randomized controlled trials assessing the safety and efficacy of Oritavancin in patients with endovascular infections, bone and joint infections and other deep-seated infections.
5. Conclusion
Oritavancin is a valuable anti-gram positive antimicrobial therapeutic with potential use in invasive and deep-seated Gram-positive infections and not only bacterial skin and soft tissue infections. Its value rest in the broad-spectrum Gram-positive coverage, safety profile and convenience of administration. However, randomized clinical trials are needed to compare with the standard of care therapy.
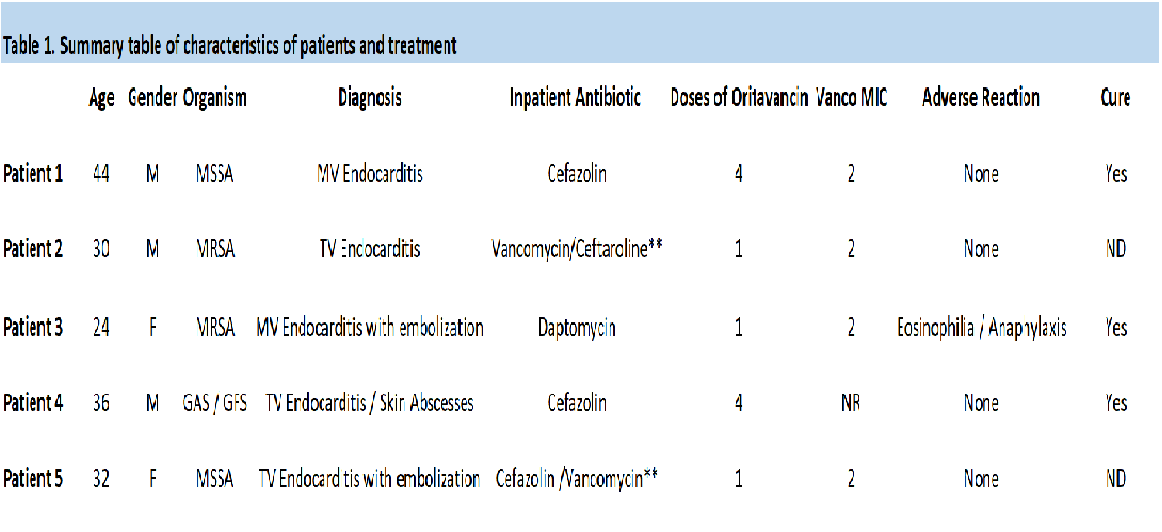
Table 1: Summary table of characteristics of patients and treatment.

 case series
case series