Sjögren’s Syndrome: A Brief Review to Newly Qualified Dentists
Shoukat Ashiti*
International Fellow in Oral Surgery at James Cook University Hospital, Middlesbrough, UK
*Corresponding author: Shoukat Ashiti, International Fellow in Oral Surgery at James Cook University Hospital, Middlesbrough, UK
Received Date: 27 October, 2022
Accepted Date: 04 November, 2022
Published Date: 08 November, 2022
Citation: Ashiti S (2022) Sjögren’s Syndrome: A Brief Review to Newly Qualified Dentists. J Surg 7: 1615. DOI: https://doi.org/10.29011/2575-9760.001615
Introduction
The term “dry mouth” has been used as either a description of an objective finding called salivary hypofunction, or a subjective description of a patient’s sensation called xerostomia. [1,2] In the last 20 years, it has been found that the occurrence of xerostomia is about 10% among people over age 50 and 40% for people over age 65.[3] Sicca complaints are very common and require various tests to reach a diagnosis. The most common causes of dry mouth are 1) xerogenic drugs such as antihistamines, antihypertensives, antidepressants, diuretics and antipsychotics; 2) radiotherapy to the head and neck; 3) Sjögren’s Syndrome (SS); 4) connective tissue diseases such as Rheumatoid Arthritis (RA), Systemic Lupus Erythematosus (SLE) and systemic sclerosis; 5) HIV or chronic active hepatitis. [4]
Assessment
History and Examination
Firstly, a thorough history including the chief complaint, dental problems, medical history and medications should be taken. In the presence of SS, extraoral examination may reveal glandular (salivary or lacrimal) enlargement which may exhibit firm, diffuse and non-tender enlargement. Additionally, the patient should be examined for any angular cheilitis as it is a common sign caused by xerostomia [5-7] .Figure 1. Intraoral examination would assess 1) the dryness of the mucous membranes; 2) dry lips; 3) touch sensitivity response to dental instruments; 4) any dental cervical margin caries; 5) absent or cloudy saliva expressible from the parotid or submandibular duct; 6) overgrowth of Candida species producing oral erythema; 7) hyperlobulated tongue with loss of filiform papillae [5,6]. Sublingual salivary pooling can be examined by drying under the tongue and monitoring salivary secretion over a minute. Abundant secretion of saliva is strong evidence against salivary hypofunction [7] Figure 1.

Figure 1: Oral signs of salivary gland dysfunction in Sjögren’s syndrome. [8] A. Dryness of the lips and marginal caries B. Dryness of the mucosa intraorally. C. Extreme desiccation of the tongue with depapillation. D. Caries on the cusp tips. E. Chronic enlargement of the major salivary glands (arrows).
Initial eye evaluation is equally as important and should check for any 1) irritation or discomfort which may be described by the patient as burning or stinging sensation; 2) dryness; 3) redness of the conjunctiva; 4) ocular fatigue; 5) photosensitivity. [9] In addition, the patient might be examined for sensory peripheral neuropathy as it is common among patients with SS and is associated with the presence of anti-Ro and anti-La.[10]
The patient should be asked about her physical capacity as it has been found that women with pSS have experienced muscle weakness and fatigue.[11]
Differential Diagnosis
After ruling out all the systemic diseases and medications that could cause sicca symptoms, a provisional diagnosis of SS can be made. SS is a chronic systemic autoimmune disorder of the exocrine glands with associated lymphocytic infiltrates of the affected glands and epithelia. [12,13] It is estimated to be the second most common immune disease after Rheumatoid Arthritis (RA) among the group of rheumatic diseases. The estimated prevalence of SS ranges between 0.5% and 1.56%, based on the diagnostic criteria, with a female to male ratio of 9:1. SS is most commonly diagnosed in the age groups 20-30, and after menopause in the mid-50s. [14-17] SS can present alone which is called primary Sjogren syndrome (pSS) or may occur in conjunction with another rheumatic disease such as RA, SLE or progressive systemic sclerosis. In this case it is called secondary Sjogren syndrome (sSS).[14,18,19] Clinical manifestations of SS can vary considerably from mainly xerostomia (dry mouth) and keratoconjunctivitis sicca (dry eyes) to developing severe systemic complications such as vasculitis, glomerulonephritis, a host of neurological manifestation and 5% of patients may develop lymphoma.[12,13,20] The aetiology of SS is unknown, however there are a few studies suggesting that SS shows class 2 Major Histocompatibility Complex (MHC) genes which is a genetic risk factor for the development of autoimmune diseases and could be involved in SS [21,22].
While others found that Human Leukocytes Antigen (HLA) class 2 markers HLA-A1, -B8, or -DR3/DQ3 haplotypes in white patients are linked to susceptibility to SS [16]. However, it has been found that the relationship between HLA and SS is restricted to patients holding anti-SSA and/or anti-SSB antibodies. [22] Additional studies been published concerning the role of some viruses such as Epstein-Barr virus, Hepatitis C virus, human T-cell leukemia and HIV; however, no single specific virus has been shown to be closely involved. [23,24] The pathophysiology of SS has been extensively studied and it has been found to be multifactorial and thought to involve immunological, hormonal, genetic and viral components. [25] Immunologically, it is found that immune cells, both cytokines and chemokines have an important role systemically and locally in the salivary and lacrimal glands, the main organs for the disease. [26] Patients with pSS have an activated type 1 interferon (INF), which are cytokines interfering with virus infections. It has been suggested that INF contributes to breakdown of tolerance and stimulation of an autoimmune response, however the critical steps of the mechanism behind INF in relation to SS are unknown. Production and action of interferon-α in SS can be seen in Figure 2 [23,27].
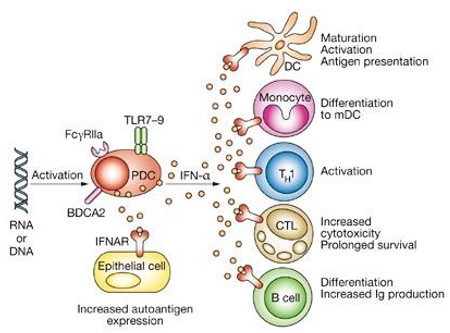
Figure 2: Activated Plasmacytoid Dendritic Cells produce interferon-α that acts on the interferon-α/β receptor. Interferon-α has pleiotropic activating effects on the adaptive immune system and increases the expression of Ro52 autoantigen in salivary gland epithelial cells. [23]
Other studies have shown that anti-Ro- and anti-La- producing B-cells were presented in the lymphocytic infiltrates of the affected glands. It has been thought that those cells are affecting glands’ function by: 1) secretion of cytokines; 2) production of auto-antibodies that interfere with muscarinic receptors; 3) secretion of metalloproteinases that interfere the interaction between the glandular cell and extracellular matrix. [28,29] However, some advocate that hormones such as oestrogen may be the main cause of difference in incidence between men and women. It has strong effects on auto-immune diseases and it is essential for initiation of autoimmunity. [30] Oestrogen expressions play a role in specific cellular sensitivity to female hormones. Females produce higher immunoglobulin at base line and in response to infection or immunisation compared to males.[31] Additionally, androgens may protect from autoimmunity and it has been found that women with SS have androgen deficiencies. [32] However, the following conditions could mimic SS because of their potential effect on both lacrimal and salivary gland; Table 1.
|
Condition |
How to be distinguished from SS |
|
Age-related sicca syndrome |
Evidence of immune system disease (anti-Ro/SSA and anti-La/SSB) are usually negative in those patients. |
|
IgG4-related disease |
By clinical and laboratory features and the distinct histopathologic findings seen in IgG4-RD. |
|
Benign lymphoepithelial sialadenitis and dacryoadenitis |
It has the histopathology characteristic of advanced SS, which are islands of epithelial cells within lymphoid infiltrate of the ductal epithelium. Patients can be defined during the evaluation of salivary gland enlargement. |
|
Lymphoma and other hematologic malignancy |
Malignant infiltration of the parotid may happen in both children and adults. It presents with bilateral salivary and lacrimal gland enlargement. |
|
Sarcoidosis |
Usually it can resemble SS but can be distinguished by biopsy. |
|
Hepatitis C |
Despite that clinical and immunologic findings may be similar, some histologic features may differ and symptoms of dryness may be less frequent. |
|
HIV infection |
Diffuse CD8 lymphocytosis syndrome is a manifestation of HIV infection. Salivary gland biopsies show a CD8-predominant lymphocytic infiltrate. |
|
Graft-versus-host disease |
the extent of lymphocytic infiltration was less than in SS, and patients can generally be distinguished from those with SS based upon the clinical examination. |
|
Systemic vasculitis |
Bilateral parotid and submandibular gland enlargement are rare manifestations of granulomatosis with polyangiitis (GPA). Clinical, laboratory, and histologic tests can distinguish GPA from SS. |
Table 1: Entities may mimic SS because of their potential involvement of both the lacrimal and salivary glands [7].
Classification Criteria
The diagnosis of SS is usually difficult and requires a multidisciplinary approach, because sicca symptoms are common, non-specific and there is no gold standard diagnostic test. [33] The diagnosis is usually made retrospectively when patients experience more severe complications than sicca such as vasculitis, arthritis, parotitis, etc. [16] However, there is a disagreement among physicians about the diagnostic criteria of SS. As in patients with milder sicca symptoms and less characteristic antibody profiles, diagnosis and therapy are difficult. [14]. Many sets of classification criteria have been proposed in the last fifty years. The 2002 revised American-European Consensus Group (AECG) classification criteria have had widespread acceptance and adoption in clinical application and studies of SS. The AECG criteria consist of six criteria, two subjective and four objective. [33] Table 2.While, in 2012 the American College of Rheumatology (ACR) declared a new set of preliminary criteria proposed by the Sjögren's International Collaborative Clinical Alliance (SICCA). They are focused on three objective features. [34] Table 2. Studies showed that both criteria have a similar performance among patients and there was no clear evidence for increased value of ACR over the AECG from clinical or biological perspectives. [33,35] In 2016, ACR and the European League Against Rheumatism (EULAR) developed and validated an international consensus of data-driven classification criteria for pSS. It has both common characters of ACR and AECG. [16,36,37] It eliminates the performing of salivary gland scintigraphy and parotid sialography. It clarifies the autoantibody role to include only anti-Ro/SSA antibodies and incorporates the new SICCA ocular surface staining scoring scheme, designed for ocular surface examination that use both fluorescein and lissamine green as ocular surface dyes. [7] The ACR/EULAR criteria is based on a weighted scoring system; it applies to any individual who meets the inclusion criteria, exclusion criteria and has a score of ≥4 on the weighted score system. [7,37] Table 3.overlap between five conditions in the exclusion criteria for AECG and ACR/EULAR. These are (past head and neck radiation treatment, Hepatitis C infection, AIDS, sarcoidosis, GvHD). The conditions which differ in the exclusion criteria are pre-existing lymphoma and use of anticholinergic drugs (since a time shorter than 4-fold the half-life of the drug) in AECG, and Amyloidosis and IgG4-related disease in ACR/EULAR [33,38].
|
Inclusion Criteria |
AECG |
ACR |
|
I. Ocular symptoms; |
1- have you had daily or persistent troublesome dry eyes for more than 3 months? |
None |
|
II. Oral symptoms; At least one positive answer |
1- have you had a daily feeling of dry mouth for more than 3 months? |
None |
|
III. Ocular signs; objective evidence, a positive result for at least one of the following two tests |
1- Schirmer's I test, performed without anaesthesia (≤5 mm in 5 min). 2- Rose Bengal score or other ocular dye score (≥4 according to van Bijsterveld's scoring system) |
Keratoconjunctivitis sicca with ocular staining score ≥3 (patient is not currently using daily eye drops for glaucoma and has not had corneal surgery or cosmetic eyelid surgery in the last 5 years) |
|
IV. Histopathology; |
Minor salivary gland biopsy showing focal lymphocytic sialadenitis, with a focus score ≥1. |
Labial salivary gland biopsy exhibiting focal lymphocytic sialadenitis with a focus score ≥1 focus/4 mm2 |
|
V. Salivary gland involvement; objective evidence, a positive result for at least one of the following tests |
1- Unstimulated whole salivary flow (≤1.5 mL in 15 min). 2- Parotid sialography showing the presence of diffuse sialectasis (punctate, cavitary or destructive pattern), without evidence of obstruction in major ducts. 3- Salivary scintigraphy; showing delayed uptake, reduced concentration and/or delayed excretion of tracer. |
None |
|
VI. Autoantibodies; presence in the serum of the following autoantibodies: |
Antibodies to Ro (SSA) or La (SSB) antigens, |
Positive serum anti-SSA/Ro and/or anti-SSB/La or (positive rheumatoid factor and ANA titre ≥1:320) |
|
Classification rules |
1. Patients without any potentially associated disease are diagnosed with primary SS; |
Patients who have at least 2 of the 3 objective features previously described would be described with SS. Eliminated the distinction between primary and secondary forms of SS |
Table 2: Illustration of AECG and ACR classification criteria [13,16,33,34,36,39].
|
Item |
Weight/score |
|
Labial salivary gland with focal lymphocytic sialadenitis and focus score of ≥1 foci/4 mm2 |
3 |
|
Anti‐SSA/Ro positive |
3 |
|
Ocular Staining Score ≥5 (or van Bijsterveld score ≥4) in at least 1 eye |
1 |
|
Schirmer's test ≤5 mm/5 minutes in at least 1 eye |
1 |
|
Unstimulated whole saliva flow rate ≤0.1 ml/minute |
1 |
Table 3: The ACR/EULAR weighted score system [7,37].
Investigations
Patients should be asked the aforementioned screening questions and should undergo the required tests based on the chosen diagnostic criteria:Sialometry; it is the measurement of salivary flow in two ways. First, the collection of whole saliva which is the common method because it is straightforward, requiring only a few minutes, without the need for any special equipment. However, it does not detect any salivary gland dysfunction or gland specific sialochemical changes and only a reduced rate of unstimulated whole saliva is considered as a diagnostic tool for SS. Secondly, the collection of glandular saliva which may reveal hyposecretion of specific salivary glands, and sialochemistry of the collected saliva may show changes in electrolytes and proteins reflecting the autoimmune invasion on the secretory cells. [40,41] Schirmer's I test; it was introduced in 1903 and includes the use of Whatman 41 special strip placed in the lower eyelid. It measures the basal tear secretion with the conjunctival-lacrimal trigeminal reflex.[42] Rose Bengal or other ocular dye score: its ocular surface staining patterns help in defining dry eye and gauge severity. It concentrates in corneal and conjunctival cells that lack a healthy mucin barrier.[43] Minor salivary gland biopsy showing focal lymphocytic sialadenitis: it is the number of lymphocytic foci (which are adjacent to normal-appearing mucous acini and contain more than 50 lymphocytes) per 4 mm2 of glandular tissue. [33] Figure 3.
Figure 3: Minor salivary gland biopsy from a patient with SS. Multiple lymphocyte foci are prominent and seen around glandular ducts (arrow) [23].
Management
Treatment of SS is mainly symptomatic and is directed toward controlling sicca complications as early as possible. It focuses on damage resulting from corneal ulcerations and chronic xerostomia. However, currently there are no evidence-based therapeutic guidelines. [18] Therefore, in the last thirty years the treatment of SS was limited to the use of substitute agents for sicca symptoms, glucocorticoids and immunosuppressive agents.[44] The treatment of dry eyes primarily focuses on alleviation of symptoms, which may include replacement therapy, local stimulators of tear secretion and anti-inflammatory agents. [45] Artificial tears would be used alone as first-line therapy. The patient is already using Viscotears which are polyacrylic artificial tears - clear liquid gel with high viscosity. It has longer ocular time retention compared to polyvinylalcohol. That may relieve the symptoms of dry eyes. [46] In severe dry eyes symptoms, topical ciclosporin showed to be efficient in treating various ocular surface disorders particularly dry eyes and severe allergic keratoconjunctivitis.[47] Additionally autologous serum eye drops showed potential advantage over traditional lacrimal substitutes, however studies found that there was some benefit in the short-term but no evidence of an effect after two weeks of treatment [48].
The treatment of dry mouth is mainly palliative despite that some medications have been shown to be effective. Salivary substitutes and hydration of oral tissue are considered the first-line therapy. [16] There are a wide variety of preparations as saliva substitutes, in the form of gel, sprays or oils, all can improve lubrication and protection from noxious environmental agents. Studies found that oxygenated glycerol triester spray is more effective than electrolyte spray. However, saliva substitutes are not generally accepted by patients as they are short-lived and unappetising, whereas oral moisturising gels last longer and are suitable for bedtime. [18,49] It has been found that chewing gum increased salivary production and may be preferred by patients, however there is no evidence showing that gum is better or worse than saliva substitutes.[49] Regarding non-pharmacological alternatives, there is little evidence to support the effectiveness of electrostimulation devices or acupuncture therapy on dry mouth symptoms. [50] Studies have shown that systemic agents as cholinergic drugs (pilocarpine, cevimeline) which stimulate tear and saliva secretion are effective in relieving sicca symptoms, increasing salivary production and improving subjective and objective parameters. [44,45,51] As well, Omega-3 supplements were seen to help in improving salivary flow and ocular symptoms. [52,53] Clinically it has been found that cholinergic drugs are safe, well tolerated with no serious side effects or drug-to-drug interactions of concern, however it is best to avoid them in patients with respiratory diseases and those who are taking antihypertensives. [54]
However, there is insufficient evidence to determine that other medications such as corticosteroids, methotrexate and rituximab are effective in the treatment of sicca symptoms. [53,55-57] Dental care including frequent regular dental check-ups and office and home fluoride application is essential to prevent any further caries and to detect any oral candidiasis or angular cheilitis. [45,53] The best recommended treatment for fatigue symptoms was found to be exercise and attention to diet, which provide the same benefit seen in patients with RA, SLE or multiple sclerosis. [53]
Monitoring and follow-up
Firstly, a detailed explanation of symptoms of the disease should be given to patients, which may facilitate keeping symptoms under control. Regular follow-up is essential to manage any systemic manifestations/extra glandular complications such as anaemia, renal tubular acidosis and peripheral or autonomic neuropathy and malignant lymphoma [16].
Conclusion
The difficulty of diagnosing SS comes from the fact that patients present with vague symptoms which could attributed to a range of causes. Unfortunately, it can take a long time and several visits to a range of clinicians before the patient is correctly diagnosed. It is important to remember that the oral cavity can reveal many signs about an underlying systemic condition, whereas, dentists may not consider asking patients about any other systemic manifestations and solely focus their history taking on oral problems. Until the precise aetiology is known, management may be limited to symptomatic relief. Monitoring and follow-up is vital in detecting any potential serious complications of SS.
References
- Furness S, Bryan G, McMillan R, Worthington HV (2013) Interventions for the management of dry mouth: non‐pharmacological interventions. Cochrane Database of Systematic Reviews 2013.
- Hopcraft MS, Tan C (2010) Xerostomia: an update for clinicians. Australian Dental Journal 55: 238-44.
- Billings RJ, Proskin HM, Moss ME (1996) Xerostomia and associated factors in a community-dwelling adult population. Community Dentistry and Oral Epidemiology 24: 312-316.
- Ying Joanna ND, Thomson WM (2015) Dry mouth – An overview. Singapore Dental Journal 36: 12-17.
- Daniels TE (1987) Oral Manifestations of Sjögren’s Syndrome. In: Talal N, Moutsopoulos HM, Kassan SS, editors. Sjögren’s Syndrome: Clinical and Immunological Aspects. Berlin, Heidelberg: Springer Berlin Heidelberg 1987: 15-24.
- Fidalgo TKdS, Nogueira C, Andrade MRTC, Valente AGLR, Tannure PN (2016) Oral Rehabilitation and Management for Secondary Sjögren's Syndrome in a Child. Case reports in dentistry 2016: 3438051.
- Baer A (2016) Diagnosis and classification of Sjögren’s syndrome. UpToDate, Waltham 2016.
- Fox PC, Brennan M, Pillemer S, Radfar L, Yamano S, et al. (1998) SJOÖGREN'S SYNDROME: A MODEL FOR DENTAL CARE IN THE 21ST CENTURY. The Journal of the American Dental Association 129: 719-728.
- Akpek EK, Amescua G, Farid M, Garcia-Ferrer FJ, Lin A, et al. (2018) Dry Eye Syndrome Preferred Practice Pattern. the American Academy of Ophthalmology 2018.
- Scofield AK, Radfar L, Ice JA, Vista E, Anaya J-M, et al. (2012) Relation of sensory peripheral neuropathy in Sjögren syndrome to anti-Ro/SSA. J Clin Rheumatol 18: 290-293.
- Strömbeck B, Ekdahl C, Manthorpe R, Jacobsson LTH (2003) Physical capacity in women with primary Sjögren's syndrome: A controlled study. Arthritis Care & Research 49: 681-688.
- Virdee S, Greenan-Barrett J, Ciurtin C (2017) A systematic review of primary Sjögren's syndrome in male and paediatric populations. Clinical rheumatology 36: 2225-2236.
- Patel R, Shahane A (2014) The epidemiology of Sjögren's syndrome. Clinical epidemiology 6: 247-255.
- Fox RI (2005) Sjögren's syndrome. The Lancet 366: 321-331.
- Kabasakal Y, Kitapcioglu G, Turk T, Öder G, Durusoy R, et al. (2006) The prevalence of Sjögren's syndrome in adult women. Scandinavian Journal of Rheumatology 35: 379-383.
- Sjogren syndrome. BMJ : Best Practice 2018.
- Bowman SJ, Ibrahim GH, Holmes G, Hamburger J, Ainsworth JR (2004) Estimating the prevalence among Caucasian women of primary Sjogren's syndrome in two general practices in Birmingham, UK. Scand J Rheumatol 33: 39-43.
- Kassan SS, Moutsopoulos HM (2004) Clinical Manifestations and Early Diagnosis of Sjögren Syndrome. Archives of Internal Medicine 164: 1275-1284.
- Drosos AA, Venetsanopoulou AI, Siozos C, Tsifetaki N, Voulgari PV, et al. (2005) Epidemiology of primary Sjögren's syndrome in north-west Greece, 1982–2003. Rheumatology 45: 187-191.
- Nocturne G, Mariette X (2013) Advances in understanding the pathogenesis of primary Sjögren's syndrome. Nature Reviews Rheumatology 9: 544.
- Tsunawaki S, Nakamura S, Ohyama Y, Sasaki M, Ikebe-Hiroki A, et al. (2002) Possible function of salivary gland epithelial cells as nonprofessional antigen-presenting cells in the development of Sjögren's syndrome. The Journal of Rheumatology 29: 1884-1896.
- Gottenberg J-E, Busson M, Loiseau P, Cohen-Solal J, Lepage V, et al. (2003) In primary Sjögren's syndrome, HLA class II is associated exclusively with autoantibody production and spreading of the autoimmune response. Arthritis & Rheumatism 48: 2240-2245.
- Nordmark G, Alm GV, Rönnblom L (2006) Mechanisms of Disease: primary Sjögren's syndrome and the type I interferon system. Nature Clinical Practice Rheumatology 2: 262.
- James JA, Harley JB, Scofield RH (2001) Role of viruses in systemic lupus erythematosus and Sjogren syndrome. Current opinion in rheumatology 13: 370-376.
- Nocturne G, Mariette X (2013) Advances in understanding the pathogenesis of primary Sjogren's syndrome. Nature reviews Rheumatology 9: 544-556.
- Dorner T, Lipsky PE (2002) Abnormalities of B cell phenotype, immunoglobulin gene expression and the emergence of autoimmunity in Sjogren's syndrome. Arthritis research 4: 360-371.
- Samuel CE (2001) Antiviral actions of interferons. Clinical microbiology reviews 14: 778-809.
- Fox PC (2007) Autoimmune Diseases and Sjögren's Syndrome. Annals of the New York Academy of Sciences 1098: 15-21.
- Lemp MA (2005) Dry Eye (Keratoconjunctivitis Sicca), Rheumatoid Arthritis, and Sjögren’s Syndrome. American Journal of Ophthalmology 140: 898-899.
- Whitacre CC (2001) Sex differences in autoimmune disease. Nature immunology 2: 777-780.
- Ackerman LS (2006) Sex hormones and the genesis of autoimmunity. Archives of dermatology 142: 371-376.
- Sullivan DA, Belanger A, Cermak JM, Berube R, Papas AS, et al. (2003) Are women with Sjogren's syndrome androgen-deficient? J Rheumatol 30: 2413-2419.
- Rasmussen A, Ice JA, Li H, Grundahl K, Kelly JA, et al. (2014) Comparison of the American-European Consensus Group Sjögren's syndrome classification criteria to newly proposed American College of Rheumatology criteria in a large, carefully characterised sicca cohort. Annals of the Rheumatic Diseases 73: 31.
- Shiboski S, Shiboski C, Criswell L, Grundahl K, Kelly J, et al. (2012) New classification criteria for Sjögren's Syndrome: a data-driven expert-clinician consensus approach within the SICCA Cohort. Arthritis Care Res 64: 475-487.
- Hernández-Molina G, Avila-Casado C, Nuñez-Alvarez C, Cárdenas-Velázquez F, Hernández-Hernández C, et al. (2014) Utility of the American–European Consensus Group and American College of Rheumatology Classification Criteria for Sjögren’s syndrome in patients with systemic autoimmune diseases in the clinical setting. Rheumatology 54: 441-448.
- Douglas L (2018) Facilitating timely diagnosis of Sjögren's syndrome. Bdj Team 5: 18026.
- Shiboski CH, Shiboski SC, Seror R, Criswell LA, Labetoulle M, et al. (2017) 2016 American College of Rheumatology/European League Against Rheumatism Classification Criteria for Primary Sjögren's Syndrome: A Consensus and Data-Driven Methodology Involving Three International Patient Cohorts. Arthritis & rheumatology (Hoboken, NJ) 69: 35-45.
- Le Goff M, Cornec D, Jousse-Joulin S, Guellec D, Costa S, et al. (2017) Comparison of 2002 AECG and 2016 ACR/EULAR classification criteria and added value of salivary gland ultrasonography in a patient cohort with suspected primary Sjögren's syndrome. Arthritis Res Ther 19: 269.
- Vitali C, Bombardieri S, Jonsson R, Moutsopoulos HM, Alexander EL, et al. (2002) Classification criteria for Sjögren's syndrome: a revised version of the European criteria proposed by the American-European Consensus Group. Annals of the Rheumatic Diseases 61: 554.
- Kalk WWI, Vissink A, Spijkervet FKL, Bootsma H, Kallenberg CGM, et al. (2001) Sialometry and sialochemistry: diagnostic tools for Sjögren's syndrome. Annals of the Rheumatic Diseases 60: 1110.
- Kalk WWI, Vissink A, Stegenga B, Bootsma H, Nieuw Amerongen AV, et al. (2002) Sialometry and sialochemistry: a non-invasive approach for diagnosing Sjögren's syndrome. Annals of the rheumatic diseases 61: 137-144.
- Serruya LG, Nogueira DC, Hida RY (2009) Schirmer test performed with open and closed eyes: variations in normal individuals. Arquivos Brasileiros de Oftalmologia 72: 65-67.
- Beckman KA, Luchs J, Milner MS (2015) Making the diagnosis of Sjögren's syndrome in patients with dry eye. Clinical ophthalmology (Auckland, NZ) 10: 43-53.
- Ramos-Casals M, Tzioufas AG, Stone JH, Sisó A, Bosch X (2010) Treatment of Primary Sjögren Syndrome: A Systematic Review. JAMA 304: 452-460.
- Mavragani CP, Moutsopoulos NM, Moutsopoulos HM (2006) The management of Sjögren's syndrome. Nature Clinical Practice Rheumatology 2: 252-261.
- Brodwall J, Alme G, Gedde-Dahl S, Smith J, Lilliedahl NP, et al. (1997) A comparative study of polyacrylic acid (Viscotears®) liquid gel versus polyvinylalcohol in the treatment of dry eyes. Acta Ophthalmologica Scandinavica 75: 457-461.
- Tatlipinar S, Akpek EK (2005) Topical ciclosporin in the treatment of ocular surface disorders. British Journal of Ophthalmology 89: 1363.
- Pan Q, Angelina A, Marrone M, Stark WJ, Akpek EK (2017) Autologous serum eye drops for dry eye. Cochrane Database of Systematic Reviews 2017.
- Furness S, Worthington HV, Bryan G, Birchenough S, McMillan R (2011) Interventions for the management of dry mouth: topical therapies. Cochrane Database of Systematic Reviews 2011.
- Furness S, Bryan G, McMillan R, Birchenough S, Worthington HV (2013) Interventions for the management of dry mouth: non‐pharmacological interventions. Cochrane Database of Systematic Reviews 2013.
- Papas AS, Sherrer YS, Charney M, Golden HE, Medsger TA, et al. (2004) Successful Treatment of Dry Mouth and Dry Eye Symptoms in Sjogren's Syndrome Patients With Oral Pilocarpine: A Randomized, Placebo-Controlled, Dose-Adjustment Study. J Clin Rheumatol 10: 169-177.
- Singh M, Papas A, Gilbard JP (2016) The Effect of an Omega-3 Supplement on Dry Mouth and Dry Eye in Sjögren's Patients. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology 106: e7.
- Vivino FB, Carsons SE, Foulks G, Daniels TE, Parke A, et al. (2016) New Treatment Guidelines for Sjögren's Disease. Rheum Dis Clin North Am 42: 531-551.
- Porter SR, Scully C, Hegarty AM (2004) An update of the etiology and management of xerostomia. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology 97: 28-46.
- Akpek EK, Lindsley KB, Adyanthaya RS, Swamy R, Baer AN, et al. (2011) Treatment of Sjögren's Syndrome–Associated Dry Eye: An Evidence-Based Review. Ophthalmology 118: 1242-52.
- Skopouli FN, Jagiello P, Tsifetaki N, Moutsopoulos HM (1996) Methotrexate in primary Sjogren's syndrome. Clinical and experimental rheumatology 14: 555-558.
- Devauchelle-Pensec V, Mariette X, Jousse-Joulin S, Berthelot J-M, Perdriger A, et al. (2014) Treatment of Primary Sjögren Syndrome With Rituximab: A Randomized Trial. Annals of Internal Medicine 160: 233-242.

 review article
review article