Successful Intra-Arterial Thrombolysis and Stenting in an Acute Ischemic Stroke Patient Caused by Anterior Cerebral Artery (ACA) Dissection with Occlusion
Yufei Liu, Yiran Zhou, Shun Zhang, Li Li, Hongquan Zhu, Su Yan, Wenzhen Zhu*
Department of Radiology, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
*Corresponding author: Wenzhen Zhu, Department of Radiology, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, 1095 Jiefang Ave, 430030, Wuhan, China
Received Date: 09 August 2022
Accepted Date: 13 August 2022
Published Date: 17 August 2022
Citation: Liu Y, Zhou Y, Zhang S, Li Li, Zhu H, et al (2022) Successful Intra-Arterial Thrombolysis and Stenting in an Acute Ischemic Stroke Patient Caused by Anterior Cerebral Artery (ACA) Dissection with Occlusion. Ann Case Report 7: 910. DOI: https://doi.org/10.29011/2574-7754.100910
Abstract
Ischemic stroke is a major cause of death and disability in China and worldwide. Many reasons can cause stroke, including atherosclerosis, artery embolization, and cervical artery dissection and so on. Among them, spontaneous intracerebral artery dissection is a rare cause of acute ischemic stroke. Here we present a case of anterior cerebral artery (ACA) dissection with occlusion causing cerebral infarction, and successfully cured by arterial thrombolysis and stenting. A 60‑year‑old man was admitted because of ischemic stroke. Imaging examination showed that the proximal A2 segment of the right ACA was occluded, suggesting an occlusive infarction of the right anterior cerebral artery. After emergency intravenous thrombolysis, the symptoms of patient were relieved, but the symptoms aggravated again one hour later. Emergency DSA was performed, and the symptoms were improved after arterial thrombolysis and stenting. After 10 days, CT showed that the right cerebral infarction area was slightly limited than before. 1 month later, the symptoms were significantly improved, the patient could walk independently, and was discharged 42 days after the onset of the disease.
Keywords: Anterior cerebral artery dissection; Ischemic stroke; CTP; CTA; DSA; Intra-arterial thrombolysis; Stenting
Case report
A 61‑year‑old man was admitted with sudden slurred speech and left hemiparesis during work. He had sweating, nausea, vomiting, urinary incontinence and transient loss of consciousness. In the neurological examination, he presented with drowsiness, loss of speech, angulus oris slanted to right and shallower right nasolabial sulcus. Muscle strength of the left upper and lower limb was grade 0 and pathological signs of both lower limbs were positive. His initial National Institute of Health Stroke Scale (NIHSS) score was 9. His past medical history was positive for hypertension, obstructive sleep apnea syndrome (OSAS), hyperuricemia, and impaired glucose tolerance. A one-stop brain CT, CTP examination at 1 hour past symptom onset were performed on arrival. Although there was no obvious abnormality on plain CT due to the insensitivity of CT for hyperacute infarct (Figure 1a), CTP could show obvious attenuated perfusion in the area supplied by the right ACA, involving the right frontal lobe, cingulate gyrus, parietal lobe and the right side of corpus callosum. Specifically, cerebral blood flow (CBF) and cerebral blood volume (CBV) were significantly reduced (Figure 1b, 1c), while mean transit time (MTT) and time to peak (TTP) were delayed (Figure 1d, 1e) in these affected areas. The size of ischemic penumbra was 74.8 ml, which was defined as the mismatch area between CBF and CBV where CBF reduced and CBV is relative normal. While the size of core infarct was 8.0 ml, which was defined as the area where CBF and CBV both reduced (Figure 1b, 1c). CTA imaging from the CCTP data showed occlusion of the right ACA from proximal A2 segment (Figure 1f).
Figure 1: Brain CT on admission (a) There was no obvious low-density area on early CT scan, yet the arrow indicates the hyperdense anterior cerebral artery sign. (b) Cerebral blood flow (CBF) showed significantly reduced flow in right frontal lobe, cingulate gyrus, parietal lobe and corpus callosum, and cerebral blood volume (CBV) map (c) had significantly reduced blood volume. Mean transit time (MTT) and time to peak (TTP) (d+e) manifested as delayed MTT and TTP. (f) CTA revealed the A2 segment of right anterior cerebral artery was occluded (arrow)
The patient was given intravenous thrombolysis with alteplase 66 mg 100 minutes after symptom onset and the above symptoms were relieved in about 10 minutes after intravenous thrombolysis. However, the patient developed left hemiplegia and drowsiness again one hour later. Emergency digital subtraction angiogram (DSA) was subsequently performed. There was filling defect of the A2 segment of the right ACA, and a small amount of contrast agent in distal ACA (Figure 2a). Microcatheter thrombolytic therapy was given and the patency of blood flow returned to normal. Angiography from the microcatheter clearly showed the distal portions of the ACA. However, there was residue contrast agent near the A2 segment of ACA in angiography, indicating a dissection here (Figure 2b). Thereafter, a stent (Solitaire 4.0 * 20 mm) was implanted in the A1-2 segment. ACA angiography showed the false lumen of dissection almost disappeared (Figure 2c). However, the dissection was not shown on CTA images as there was not enough gathering of contrast agent in ACA during CTA (Figure 1f). The anti-platelet medicine Tirofiban, volume expansion and symptomatic support treatment was given after the operation. DWI images on the third day post symptom onset revealed obvious high signal, with reduced values (Figure 3a-c).
Figure: 2-The digital subtraction angiogram. (a) Arrow indicates proximal aspect of ACA lumen stenosis, and obstruction is nearly complete. (b) After intra-arterial thrombolysis, there is partial recanalization of the right ACA disclosing a significant local contrast retention (arrow). (c) View after placement of a stent. Arrow indicates position of proximal and distal stent markers
The patient’s symptoms slightly recovered in the next 72 hours. The CT scan on the 13rd day after symptom onset revealed limited hypodense patchy shadow in the cingulate gyrus, parietal lobe and the right corpus callosum, while the ischemic penumbra revealed by CTA recovered well (Figure 3d). The stent was clearly shown on CTA and the distal end of ACA showed uneven thin lumen (Figure 3e, 3f). The results of neurological examination 30 days after symptom onset showed that the left upper and lower limb muscle strength was grade 5. NIHSS score was 0, mRS score was 1 and MOCA score was 28. The patient was discharged on the 42rd day after symptom onset and recovered well without obvious neurological symptoms. He could ambulate more than 3000 meters without any assistive devices and had returned to work.
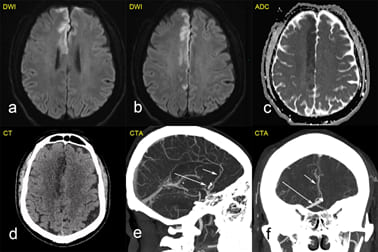
Figure 3: Post-stenting MRI at 24 hours from symptom onset and post-stenting CT at 13 days from symptom onset. The diffusion weighted image (a+b) showed high signal and the apparent diffusion coefficient image (c) showed low signal at the right frontal lobe, cingulate gyrus and parietal lobe, indicating cytotoxic edema. (d) CT showed that the penumbra brain tissue was effectively recovered, only the ischemic core area showed low-density shadow. (e+f) CTA showed the stent of A1 segment of right anterior cerebral artery (long arrow). The distal part of A3 segment was developed (short arrow) and the thickness of artery lumen was uneven.
Discussion
Spontaneous intracranial dissection is a risk factor for acute ischemic stroke [1,2]. Arterial dissection is often accompanied by arterial wall hematoma and thrombosis, which usually result in stroke in children and young adults [3]. Intracranial dissection of anterior circulation is relatively rare compared with that of vertebrobasilar system, especially in ACA [4]. ACA dissections are commonly found in unruptured form in ischemic cases, and the prognosis is usually considered to be well, only few cases of ACA dissection receiving endovascular treatment have been reported [4-6]. Spontaneous dissections were commonly located on vertebral arteries [6]. Kazuki fukuma et al. [7] reported 82 patients with ischemic stroke caused by cerebral artery dissection and ACA was involved in 12 cases. Dissection is usually related to rupture of the elastic vascular plate in the arterial wall, dissecting arteries are characterized by tearing of the internal elastic layer and media, with or without intramural hemorrhage, which leads to vascular stenosis or dilatation. After 14 days, granulation tissue causes chronic intimal thickening, repeated intramural hemorrhage and fragile neovascularization rupture. In this situation, blood enters from the break, resulting in a false lumen communicating with the true lumen [3]. ACA dissection secondary to autosomal dominant polycystic kidney disease and sildenafil have also been reported [8]. However, it is difficult to form a complete understanding of the pathogenesis and pathological process due to the limited cases. False lumen thrombosis of dissecting artery may lead to stenosis, occlusion or distal embolism of the parent artery, while hemodynamic changes may lead to watershed infarction [3,9]. In our case, the most probable cause of infarction is the occlusion of A2 segment of ACA due to the increased compression from the dissection false lumen and the thrombosis in the true lumen. To date there are no definitive guidelines for the optimal treatment of ischemic stroke resulting from thrombosis of cerebral artery dissection. The treatment and diagnosis of cerebral artery dissection thrombosis depends on limited literature [1,4-6]. Traditional treatment includes surgery and endovascular surgery to block the dissection. Recently, endovascular reconstruction, such as stent assisted embolization or shunt, has been reported to be effective [10]. On the other hand, although intravenous thrombolysis with recombinant tissue plasminogen activator (rtPA) had proven to be effective for the treatment of ischemic stroke within 4.5 hours of symptoms, onset, it still has limitations, especially for anterior circulation ischemic stroke (ACIS) [11,12]. This is further confirmed by the poor effect of emergency intravenous thrombolysis in our case. By comparison, stenting after thrombolysis is a feasible and effective treatment method to close the intimal tear because of the pathological characteristics of the dissection. Moreover, stenting has been widely used in intracranial artery dissection, and no obvious safety risk was reported [10]. How to make the diagnosis of hyperacute stage and determine the ischemic penumbra in the pathophysiological stage of acute cerebral infarction, so as to implement effective protective measures in the effective time window of brain tissue treatment, is the most important issue in the treatment of acute cerebral infarction. The CT scan of out case was negative due to the hyperacute period, although there was a suggestion of hyperdense anterior cerebral artery sign, it could not be diagnosed. However, CTP and CTA showed high sensitivity and accuracy in acute ischemic stroke [12]. When CBF decreased moderately, brain tissue swelled due to ischemia and gradually began to compress local micro-vessels. The perfusion imaging of our case showed that MTT and TTP were delayed and CBF was reduced obviously. However, CBV was basically normal or only slightly reduced at this time due to cerebral local circulation compensation. By analyzing the mismatch between CBF / MTT images and CBV images, we confirmed the existence of ischemic penumbra and guided intravenous thrombolysis in the window period [13]. One hour after intravenous thrombolysis, the symptoms of our case recurred, so the emergency DSA was performed for intra-arterial thrombolysis. Through the retention of contrast medium, the cause of the disease was confirmed as anterior cerebral artery dissection during the operation, so stenting was performed. Our case provides a good example for the diagnosis and treatment of similar cases, the significant recovery of ischemic penumbra indicates the importance of imaging guidance in stroke treatment. It also shows that the acknowledgement of potential existence of ACA dissection is of great importance for timely and accurate treatment.
References
- Lian Y, Chen X, Kong DR, Chen W, Shi MC, et al (2020) Cervical artery dissection-an easily neglected cause of stroke: a case report. BMC Neurol 20: 428.
- Park K-H, Kwak HS, Park J-S (2020) Endovascular Approach in Patients with Acute Complete Occlusion Due to Middle Cerebral Artery Dissection. Journal of Korean Neurosurgical Society 63: 717-722.
- Debette S, Compter A, Labeyrie MA, Uyttenboogaart M, Metso TM, et al (2015) Epidemiology, pathophysiology, diagnosis, and management of intracranial artery dissection. The Lancet Neurology 14: 640-654.
- Wang Y, Geng Y, Shi Z, Shi T, Zhang J (2017) Good recovery of subarachnoid hemorrhage concomitant with ischemia due to anterior cerebral artery dissection by conservative treatment: A case report. Exp Ther Med 14: 155-158.
- Lamprou V, Astreinidis A, Davidhi A, Staikoglou N, Psoma E, et al (2020) Distal middle cerebral artery dissection with concurrent completely thrombosed aneurysm manifesting as cerebral ischemia. A case report and review of the literature. Radiology Case Reports 15: 2582-2588.
- Urasyanandana K, Songsang D, Aurboonyawat T, Chankaew E, Withayasuk P, et al (2018) Treatment outcomes in cerebral artery dissection and literature review. Interv Neuroradiol 24: 254-262.
- Fukuma K, Ihara M, Tanaka T, Morita Y, Toyoda K, et al (2015) Intracranial Cerebral Artery Dissection of Anterior Circulation as a Cause of Convexity Subarachnoid Hemorrhage. Cerebrovascular Diseases 40: 45-51.
- Tanaka M, Takasugi J, Hatate J, Otsuka N, Sugiura S, et al (2019) Anterior Cerebral Artery Dissection in a Patient With Autosomal Dominant Polycystic Kidney Disease. J Stroke Cerebrovasc Dis 28: e129-e131.
- Shi J, Meng R, Konakondla S, Ding Y, Duan Y, et al (2017) Cerebral watershed infarcts may be induced by hemodynamic changes in blood flow. Neurological Research 39: 538-544.
- Marnat G, Lapergue B, Sibon I, Gariel F, Bourcier R, et al (2020) Safety and Outcome of Carotid Dissection Stenting During the Treatment of Tandem Occlusions: A Pooled Analysis of TITAN and ETIS. Stroke 51: 3713-3718.
- Koga M, Yamamoto H, Inoue M, Asakura K, Aoki J, et al (2020) Thrombolysis With Alteplase at 0.6 mg/kg for Stroke With Unknown Time of Onset. Stroke 51: 1530-1538.
- Rabinstein AA (2020) Update on Treatment of Acute Ischemic Stroke. Continuum (Minneapolis, Minn) 26: 268-286.
- Leigh R, Knutsson L, Zhou J, van Zijl PC (2018) Imaging the physiological evolution of the ischemic penumbra in acute ischemic stroke. Journal of cerebral blood flow and metabolism: official journal of the International Society of Cerebral Blood Flow and Metabolism 38: 1500-1516.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.