The Videocapsule Endoscopy Role in the Early Diagnosis of Small Bowel Melanoma Metastasis: A Particular “Coal Black” Endoscopic Appearance
by Maria Giulia Demarzo*, Ilaria Ghidotti, Giuliana Bisso, Maria Rita Badalamenti, Renato Santucci, Maria Caterina Parodi
Gastroenterology and Endoscopy Unit, Department of Surgery, IRCCS Ospedale Policlinico San Martino, Genoa, Italy.
*Corresponding author: Maria Giulia Demarzo, MD, Gastroenterology and Endoscopy Unit, Department of Surgery, Largo Rosanna Benzi n° 10 16132, Genoa, Italy.
Received Date: 24 October, 2022
Accepted Date: 7 November, 2022
Published Date: 10 November, 2022
Citation: Demarzo MG, Ghidotti I, Bisso G, Badalamenti MR, Santucci R, Parodi MC (2022) The Videocapsule Endoscopy Role in the Early Diagnosis of Small Bowel Melanoma Metastasis: A Particular “Coal Black” Endoscopic Appearance. J Dig Dis Hepatol 7: 185. DOI: https://doi.org/10.29011/2574-3511.100085
Abstract
Background: Small bowel melanoma metastasis can be very tricky to diagnose. Videocapsule endoscopy allows the exploration of the entire small bowel and might represent a very useful tool in the melanoma staging. Methods: we describe the clinical history of two male patients of 31 and 75 years old affected by melanoma. Both were admitted to the hospital for melena. Esophagogastroduodenoscopy and colonoscopy failed to show causes of bleeding. We performed videocapsule endoscopy to find the bleeding source. Results: The youngest patient had countless black or blue lesions and a big bleeding ulcer with a “coal black” depression with exophytic whitish borders (the so-called “solar eclipse”). He underwent successful jejunum resection but died for brain metastasis two months later. The second patient showed five sessile and pedunculated polypoid lesions and a peculiar extensive black ulceration surrounded by whitish area, very similar to that of the youngest patient. Small bowel resection was performed and the patient is still alive. Conclusions: Haemorrhagic small bowel melanoma metastasis seem to have a peculiar endoscopic appearance. Introducing videocapsule in the melanoma staging could lead to early diagnosis and early treatment helping to improve survival rates. Further investigations are needed to increase our knowledge in this field.
Keywords: Melanoma metastasis; Solar eclipse; Small bowel; Videocapsule endoscopy; Coal black appearance; Early diagnosis
Introduction
Melanoma has the poorest prognosis above other skin cancers. Despite the introduction of new targeted therapies, the metastatic melanoma is the leading cause (approximately 80%) [1] of skin tumours related deaths. Actually, metastasis are the most important prognostic factor of patient’s survival.
Gastrointestinal (GI) tract is a common site of malignant melanoma metastasis, they localize mainly in the small bowel followed by large bowel and stomach [2]. The symptoms include abdominal pain, nausea, iron-deficiency anaemia from GI bleeding and weight loss. Rarely, melanoma metastasis can be responsible for intussusception and bowel perforation [3].
Unfortunately, small bowel metastasis, although lifethreatening, are frequently underdiagnosed being a post mortem finding in the 60% of cases [4]. Computed Tomography (CT) scan can fail in recognize them when the mass is inferior to detectable size (1 cm) [5].
Video capsule endoscopy (VCE) is a non-invasive technique for the visualization of the entire small intestine. Unexplained anaemia from occult GI bleeding is one of the major indications for performing VCE. In metastatic melanoma patients undergoing VCE, a singular coal-black capsule endoscopic appearance of melanoma metastasis was reported [6-8]. It consists of a central coal- black depression encircled from bleached intestinal villi in a so called “solar eclipse” image. This phenomenon is probably related to the disappearance of melanocytes in the tissue surrounding the metastasis in patients undergoing therapy.
This suggest that VCE could represent a very useful tool in melanoma staging.
Hereby, we describe two clinical cases of haemorrhagic small bowel melanoma metastasis with a characteristic VCE image.
Case 1
A 31-year-old man diagnosed with malignant melanoma of the neck stage III in October 2020. He immediately underwent surgical excision with subsequent dabrafenib trametinib treatment. 10 months later the patient presented to our hospital with melaena and vertigo and he was referred to our Gastroenterology Unit for severe iron deficiency anaemia in blood tests. We performed gastroscopy and colonoscopy, but none of them have been conclusive for an active bleeding source. In the meantime, Head MRI (Magnetic Resonance Imaging) showed brain metastasis while a Total Body CT scan detected an adrenal mass. Therefore, we performed a VCE which provided evidence for numerous blue or black pigmented lesions suspicious for melanoma intestinal localization in the jejunum. Two of them were bleeding and had a characteristic coal-black appearance with a black central depression and whitish margins (Figure 1). In a few days the patient underwent a new Gastroscopy 40 cm away from the Treitz band reaching the bleeding lesions that have been marked by endoscopic tattoo and subsequently successfully resected by laparoscopic surgery. After the surgery the patient no longer needed blood transfusions. Successively he had Radiotherapy to larger brain metastasis and nivolumab 480 mg treatment was started. Unfortunately, the patient died two months later (from brain disease progression), in December 2021.
Figure 1: Characteristic coal-black VCE appearance of bleeding melanoma metastasis
Case 2
A 75 years old male patient with an already known metastatic melanoma of the right foot presented to the Emergency Room (ER) of our hospital complaining asthenia and melena in April 2022.
During the interview, the patient reported a long-standing disease with multiple treatments. At that time, he had already had IFN (interferon) at diagnosis. Two years later, he experienced lymphatic, pulmonary and adrenal disease progression and he had abdomen radiotherapy. Hence, immunotherapy with nivolumab was started. In 2021 a timely screening abdomen CT scan showed gastric metastasis; thus, he underwent partial gastrectomy.
On ER admission blood tests revealed severe anaemia (Hb 70 g/L) needing blood transfusions and the patients was just referred to our Gastroenterology Unit. Esophagogastroduodenoscopy, colonoscopy and Total Body CT scan were promptly performed, but none of these displayed any bleeding lesions. A total positron emission
tomography (PET) scan revealed an increased uptake in the ileal tract (Standardized Uptake Value 12). Subsequently, we decided to perform VCE which showed deep black partially confluent ulcers surrounded by whitish area, indicative of haemorrhagic melanoma metastasis (Figure 2), and 5 further blue and non-pigmented sessile and pedunculated polypoid (Figure 3) lesions in the jejunum as well as a Merkel diverticulum in the ileum.
We referred the patient to the surgeon consultant and a small bowel resection was performed. The surgery was deemed a success and the patient was discharged on the post-operative eleventh day. The patient keeps getting oncological therapy.

Figure 2: VCE appearance of small bowel melanoma metastasis
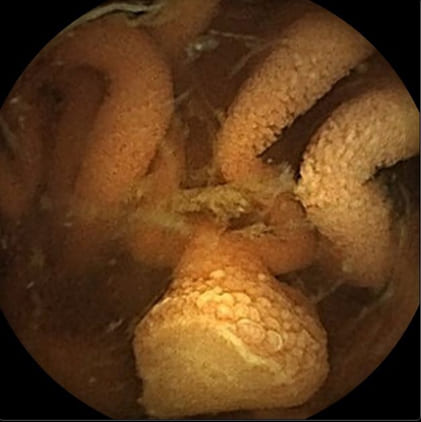
Figure 3: Polypoid small bowel melanoma metastasis
Discussion
Although rarely described, melanoma GI metastasis are more common than usually thought. The most common location is the small bowel, and the most common manifestation is iron deficiency anaemia, rarely followed by intestinal obstruction and perforation. Hence, despite being underdiagnosed, small bowel melanoma metastasis is a potentially deadly condition.
Current guidelines do not include small bowel examination in the melanoma staging. At present, VCE is only performed in case of anaemia, even if there are many patterns of melanoma metastasis and the polypoid one seems to be the most common [9]. So VCE could be very useful in melanoma patients, even in non- specific symptoms such as abdominal pain or intestinal obstruction signs. Emerging evidences in literature suggest that early diagnosis and consequently early treatment could pose in better outcomes [10-11]. We reported two cases with very different conclusions: one patient survived and the other died. Nevertheless, in both cases surgery was successful; the low survival of the first patient was
related to brain disease progression rather than intestinal metastasis. Indeed, Gallino et al. [12] showed as R0 surgery improved survival rate in small bowel metastatic melanoma regardless the presence of metastasis in other organs.
Keeping this in mind it could be worth including VCE in the melanoma cancer staging in the future. A decade after the first description, Principe et al. [6] pointed out an emblematic VCE image -meaning a coal black appearance with surrounding whitish tissue - highlighting the usefulness of VCE in metastatic melanoma.
To the best of our knowledge, these cases are the fourth and fifth of coal-black appearance intestinal melanoma metastasis ever described in literature. So far, this peculiar phenomenon shows up in patients undergoing immunotherapy. One of our two patients did not undergo immunotherapy. Further studies will be needed to clarify if the so-called “solar eclipse” is a consequence of such treatment, as hypothesized.
This leads us to two main considerations. Firstly, small bowel melanoma metastasis seems to be not so rare. Secondly, in this perspective the awareness of a characteristic endoscopic feature could lead to an early diagnosis and so help preventing complications.
Conclusions
Despite multiple case-reports in the current literature, small bowel metastasis from melanoma is largely underestimated. There are no guidelines yet for management of GI melanoma metastasis. We showed how early referral to surgery may result in positive outcomes for patients. Reporting our experience, we would like to offer our contribute on the awareness of the course of this pernicious neoplasia in order to increase evidences that early diagnosis and treatment may help improving survival rates.
References
- Aladowicz E, Ferro L, Vitali GC, Venditti E, Fornasari L, et al. (2013)Molecular networks in melanoma invasion and metastasis. Future Oncol 9: 713-726.
- Holmberg CJ, Alwan G, Ny L, Olofsson Bagge R, Katsarelias D (2019) Surgery for gastrointestinal metastases of malignant melanoma - a retrospective exploratory study. World J Surg Oncol 17: 123.
- Yagmur Y, Açıkgöz MA (2021) Metastatic melanoma causing recurrent intussusception and perforation of small bowel: case reports and literature review. Melanoma Manag 8: MMT54.
- Prakoso E, Selby WS (2007) Capsule endoscopy in patients with malignant melanoma. Am J Gastroenterol 102: 1204-1208.
- Lee MH, Zaheer A, Voltaggio L, Johnson PT, Fishman EK (2019) Clinical time course and CT detection of metastatic disease to the small bowel. Abdom Radiol (NY) 44: 2104-2110.
- Todeschini A, Loconte I, Contaldo A, Ierardi E, Di Leo A, et al. (2021) Small Bowel Metastatic Melanoma: An Emblematic “Coal-Black” Appearance at Videocapsule Endoscopy. Medicina (Kaunas) 57: 1313.
- Smedegaard J, Adamsen S (2007) Metastatic malignant melanoma of the small intestine: capsule endoscopic appearance. Endoscopy 39 Suppl 1: E209.
- Urbain D, Aerts M, Reynaert H, Mana F, Neyns B (2010) Smallbowel metastasis of malignant melanoma: video capsule endoscopy Endoscopy 42 Suppl 2: E185.
- Bender GN, Maglinte DD, McLarney JH, Rex D, Kelvin FM (2001) Malignant melanoma: patterns of metastasis to the small bowel, reliability of imaging studies, and clinical relevance. Am J Gastroenterol 96: 2392-2400.
- Malissen N, Farvacque G, Duconseil P, Birnbaum DJ, Falque C, et (2021) Surgery of small bowel melanoma metastases in the eraof efficient medical therapies: a retrospective cohort study. Melanoma Res 31: 358-365.
- Davis LE, Shalin SC, Tackett AJ (2019) Current state of melanoma diagnosis and treatment. Cancer Biol Ther 20: 1366-1379.
- Gallino G, Maurichi A, Patuzzo R, Mattavelli I, Barbieri C, et al. (2021) Surgical treatment of melanoma metastases to the small bowel: A single cancer referral center real-life experience. Eur J Surg Oncol 47: 409-415.

 case report
case report